Please note that this post is archived, with the most recent update on 4-29-22.
You can find the most recent omicron information here.
.
.
This post addresses issues specifically concerning the omicron variant. For information about Covid-19 which pertains to the delta variant, click here:
You can access archived general Covid information here:
1. How Was the US Managing Covid-19 in late 2021?
2. Do the omicron variants have different symptoms from previous SARS-CoV-2 variants? Are vaccinated people who get infected contagious?
3. How does a virus variant arise?
4. When and where did the omicron variants originate?
5. How fast have the omicron variants spread in the US? What percentage of cases occurring now are caused by them?
6. What is an R0 number in disease transmission? How has it changed from other SARS-CoV-2 variants? Why are vaccinated people getting breakthrough infections? Does that mean natural immunity is better?
7. Are the omicron variants less dangerous than the others we have seen?
8. With other variants, older people and those in poor health were most likely to have a severe case or die. Is that still true with the omicron variants?
9. What pre-exposure options are available for people who don’t develop an immune response to vaccines, like transplant patients or individuals with some blood cancers?
10. I have been exposed to SARS-CoV-2 or tested positive in the last 5–10 days. Are there safe and effective treatments available?
11. Can people who were previously infected get Covid again? How does natural immunity compare to the immunity from vaccines? Do monoclonal antibodies increase the risk of reinfection?
12. Why do the vaccines decrease the risk of hospitalization or death? How effective are they?
13. How risky is post-vaccination myocarditis for younger people? How does the risk of other vaccine side effects compare to the symptoms of Covid?
14. Are mRNA vaccines safe for pregnant women and their babies?
15. What about the risk of infertility?
16. How can I discuss this with people I love who are vaccine-hesitant?
17. What sources can I trust?
.
.
About me: I have a masters’ degree in Infectious Disease Epidemiology from UCLA, a bachelors’ degree from Wheaton College in biology with a certificate in International Community Development, and a masters’ in Greek and Hebrew Exegesis from Gordon-Conwell Theological Seminary.
Usually, I am writing and posting bible studies on the Redemptive History Facebook page, but these are not normal times. I have been writing about Covid since March 2020.
I began my career by editing a medical monograph and writing an accompanying peer-reviewed journal article during my graduate studies at UCLA (MPH, Tropical and Infectious Disease Epidemiology). My first publication concerned the excess risk of severe illness or death from a bacterium in raw milk in California. It was featured on the front page of the Los Angeles Times and was debated in the state legislature.
After graduation, I conducted records-based research concerning the efficacy of a poly-pharmacy reduction program for nursing home residents. We focused upon the frequency and severity of adverse drug reactions, and whether our patients could stop taking their medications without needing to resume using them. Textbooks still cite it today.
Paul Terrill MD, FAAFP has been an invaluable collaborator in assessing and compiling many of these resources.
.
.
Due to the sudden onset and severity of the pandemic, many journals are pre-empting their normal four-week to six-month process of peer reviewing articles before releasing them for publication. When you look at any research involving Covid-19, it is important to note the status of the article: pre-print or accepted for publication after peer review.
Check the comments under pre-print articles. Several major studies were retracted after the peer-review process detected significant issues.
Lancet, NEJM retract studies on hydroxychloroquine for COVID-19
.
.
1. How Was the US Managing Covid-19 in late 2021?
During August and September 2021, the Southeast US and Texas experienced a large wave of infections, hospitalizations, and deaths due to the delta variant. That has now shifted to the West and North, from Arizona to Montana and over to New England.
In general, we are not in a good position to be encountering a highly transmissible new variant. A darker shade in this graphic represents the amount of change in the past seven days, not how many new cases there are.
Please note that Florida updates their data on Saturdays, and the algorithm Johns Hopkins University uses does not account for that possibility. As the week progresses, the state looks better. For December 17–23, Covid cases among the state’s permanent residents increased by 323%:

The number of excess deaths in the US from all causes lags behind the spread of the omicron variant by several weeks:

JHU: Track Covid-19 Trends Across the US, See Where Cases Are Rising and Falling
Florida Covid Statistics: What is Really Happening?
CDC: Excess Deaths Associated with COVID-19
.
.
2. Do the omicron variants have different symptoms from previous SARS-CoV-2 variants? Are vaccinated people who get infected contagious?
People infected with an omicron variant are less likely to experience cough or the loss of smell. So far, the symptoms are primarily extreme fatigue, achiness, headache, and a scratchy throat instead of a sore throat. Many children infected with omicron are experiencing skin rashes. Some people remained asymptomatic.
However, this variant initially was identified in young adults, a population less likely to experience severe illness. With other variants, hospitalizations and deaths occurred approximately three weeks after diagnosis.
To see a full listing of Covid-19 symptoms, click here:
Symptoms which require immediate emergency medical care include difficulty breathing, continuous pressure or pain in the chest, an inability to awaken or to stay awake, a new onset of confusion, or a blue tinge in the face or lips.
Investing in a pulse oximeter to track your blood oxygen level is a great idea. They cost about $20. A normal oxygen saturation level runs between 95–100%. People with Covid-19 can experience a drop in that percentage without realizing it has happened. If it does occur, seek medical attention immediately.
Two of the first announced cases world-wide occurred in fully vaccinated people staying in a quarantine hotel in Hong Kong, with one person getting sick a week before the other. Both had large numbers of viral particles in their nasal swabs. They were in rooms across from each other. Over one-fourth of environmental samples taken in their rooms and the corridor tested positive for the omicron variant.
Even vaccinated people who get infected with an omicron variant can transmit the virus, especially in households with members who have not been vaccinated.
CDC: Science Brief Omicron (B.1.1.529) Variant
The Hill: Doctor Who Discovered Omicron Explains the Symptoms to Watch Out For
The Hill: Experts Say You Should Watch for an Unusual Omicron Symptom in Kids
Hong Kong Government: Analysis of Imported Cases
.
.
3. How does a virus variant arise?
Random mutations occur due to errors in the viral replication process. While coronaviruses have an enzyme which corrects most of those mistakes, some do still slip through to create a new variant. Only those mutations which confer an advantage to viral replication, transmission, or survival of immune systems expand in a host population. Since mutations are random, vaccine developers cannot predict in advance what a virus will look like in the future.
JAMA: Genetic Variants of SARS-CoV-2—What Do They Mean?
.
4. When and where did the omicron variants originate?
Originally called B.1.529, the omicron variant was initially identified in South Africa on November 24, 2021, from a sample taken almost two weeks earlier. It appears to have arrived in the US that month.
Mayo Clinic maintains a list of the variants of greatest concern world-wide.
Most omicron subvariants also appear to have arisen in South Africa. The strains which evolved from BA.2.12 were first detected in the Northeastern US.
CDC: About Variants of the Virus that Causes COVID-19
Mayo: COVID-19 Variants: What’s the Concern?
MedPage: No Real-World Evidence BA.2 Is More Severe
CDC: SARS-CoV-2 Variant Classifications and Definitions
.
5. How fast has the omicron variant spread in South Africa and in the US?
During the week of November 15–22, South Africa experienced an astounding 740% increase in Covid-19 cases (3,500 to over 29,000).
The first omicron case in the US was identified on December 1st. By December 3rd, it was identified in ten states. At least one of the patients had not traveled to South Africa, indicating it was already spreading in that community.
The CDC’s interactive dashboard shows the proportion of each variant over time for the entire US and for each region. It is currently updated every week, with update on January 29th showing 99.9% of samples consisted of the omicron variants.
It had reached 98% in only five weeks after omicron was first detected in the US. The delta variant had spread for sixteen weeks before it accounted for 98% of Covid cases (April 24th–August 14th).
A newer subvariant called BA.2 was first detected in the US on January 15th. By March 26th, it had become the dominant variant in the US. It is now being displaced by the BA.2.12.1 strain which evolved from it:

By scrolling down on that CDC site, you can see the proportions of each subvariant by region of the US on April 23, 2022.
Data for individual states is lagging by about a month:

WHO: Country Data South Africa
CDC: Science Brief Omicron (B.1.1.529) Variant
.
.
You can see what was happening in any state or county in the US yesterday compared to eight days ago. Some states report information to the CDC only twice a week.
While my focus is updating statistics for Florida on a weekly basis, you can search the links I post for other states in the US.
This map shows the level of Covid transmission in the US by county on April 28, 2022:

CDC: COVID-19 Integrated County View
Florida Covid Statistics: What is Really Happening?
.
.
6. What is an R0 number in disease transmission? How has it changed from other SARS-CoV-2 variants? Why are vaccinated people getting breakthrough infections? Does that mean natural immunity is better?
An R0 (“R naught”) represents the basic reproduction rate of a pathogen: how many people become infected when exposed to a single case. When an R0 is larger than 1.0, an outbreak is increasing; when it is less than 1.0, an epidemic is waning. Human behavior and the properties of an infectious agent both impact disease transmission, so some variability does exist.
Researchers use the R0 to estimate the proportion of a population that must no longer be susceptible to infection to reach herd immunity. That can typically be achieved by a combination of surviving natural infection and immunization. Diseases with a higher R0 require more people with immunity for transmission to stop.
The first omicron variant (B.1.1.529) spreads four times as easily as the original SARS-CoV-2 virus. The first strain of SARS-CoV-2 which came from China had an R0 of 2.5; in the UK, the delta variant was almost three times more transmissible with an R0 of approximately 7, and the R0 of omicron B.1.1.529 is 10.
Omicron BA.2 transmits 30% more easily than its predecessor, giving it an R0 of 13.
According to the New York Department of Health, the newer strains which have evolved from BA.2 are even 25% more transmissible than BA.2, yielding an R0 of 16.
A technical briefing from the UK indicates that household contacts of a person infected with omicron BA.2 become infected 20% of the time. That is double the rate from the delta variant.
CDC Emerg Inf Dis: Complexity of the Basic Reproduction Number (R0)
Lancet: Lifting of COVID Restrictions in the UK and the Delta Variant
CDC: Rates of COVID-19 Cases and Deaths by Vaccination Status
MedPage: BA.2 Blitzes Through Households, Even More than Original Omicron
.
.
For other variants, two weeks after vaccination, the antibody level of saliva from people vaccinated with either mRNA vaccine is comparable to that of people who have recovered from Covid.
That does not include the one-third of people who tested positive for SARS-CoV-2 and were sick who showed no antibody response three weeks after they felt better. Some of them were severely ill. This happened most often in younger adults.
In England, a population-based study revealed that those with a prior Covid infection were five times more likely to become infected with omicron compared to reinfection with other variants. The researchers estimate that only one-fifth of unvaccinated people who previously tested positive can fend off the omicron variant.
After several months, a comparison of antibody levels in Moderna and Pfizer recipients revealed over twice the number of antibodies produced by the Moderna vaccine. This is likely due to the increased amount of mRNA in Moderna and the longer interval between doses.
Furthermore, the two vaccines stimulate different parts of the immune system. As a result, mixing vaccine types will give you the best protection. If you had 2 or 3 Moderna, I recommend getting a Pfizer and vice versa.
Inside Medicine: The Omicron Paradox: If It’s Milder, Why Are Hospitals on the Brink of Disaster?
JAMA: Comparison of SARS-CoV-2 Antibody Response Following Vaccination with BNT162b2 and mRNA-1273
Emerg Inf Dis: Predictors of Nonseroconversion after SARS-CoV-2 Infection
.
.
The omicron variant has about 30 mutations in its spike protein. That enables escape from vaccines and from antibodies derived from natural infection.

The BA.2 subvariant has an additional 25 mutations.
Compare an antibody to a master key for a large building: it can fit into many locks with similar—but not necessarily identical—ridge patterns. If someone installs a new lock too different from the existing ones, the master key will not fit well enough to work.
Following vaccination or natural infection, when we are exposed to the virus, our circulating antibodies attach to the spike protein of SARS-CoV-2, preventing the virus from entering a cell. When there are more viral particles than available antibodies, the virus breaks through our defenses. How we behave has an enormous impact on the amount of virus we encounter.
Once inside, the omicron variant reproduces so rapidly that it can spread before our immune system has time to react, enabling the virus to spread to others. However, the vaccines also produce T cell immunity. Our T cells go on a search and destroy mission, killing any infected cells and neutralizing the virus within them. This significantly shortens how long vaccinated people can spread the virus.
People who are fully vaccinated produce more antibodies and a much stronger T cell response than those infected with SARS-CoV-2 one year ago.
In a study of omicron-specific T cells, individuals who were infected with the virus over a year ago and received two doses of the Pfizer vaccine showed a greater T cell response than those who had Covid six weeks earlier. However, compared to the original strain, T cell responses declined by 25–30% when presented with the omicron variant.
WaPo: Understanding Omicron’s Many Mutations
.
.
In mid-March 2022, people who had completed a vaccine series and booster dose were half as likely to have a positive test than unvaccinated Americans.
That was a significant decrease from February, when unvaccinated Americans had three times the number of positive tests. Waning immunity and the shift to newer subvariants accounts for this:

According to a Danish study, the newer form of omicron called BA.2 is one-third more transmissible than the original omicron variant (BA.1). It was first detected on Denmark on December 5. By the second week of January, it accounted for 45% of SARS-CoV-2 cases in that nation. It does not appear to cause more severe illness.
Compared to BA.1, the new subvariant creates illness 2x as often in unvaccinated people, 2.5x more in fully vaccinated populations, and 3x as often in those with booster shots. Applying those statistics to the specific information from the graph above, we have a chart that looks like this:

Vaccinated and boosted people continue to have substantially more protection against infection.
There are reports of people who had omicron BA.1 becoming infected with omicron BA.2. Of the 2,000,000 Danes who tested positive for omicron, only 67 of them were reinfections with another form of omicron.
This analogy by Dr. Leana Wen is helpful: “Think of the vaccine as a very good raincoat. It keeps you dry in a drizzle. If there are constant thunderstorms, you may get wet. The problem isn’t the raincoat—it’s the weather. To best protect all of us, we need to reduce the storm of Covid-19 by increasing vaccination rates.”
CDC: Rates of COVID-19 Cases and Deaths by Vaccination Status
MedRxiv: Occurrence and Significance of Omicron BA.1 Infection Followed by BA.2 Reinfection
.
.
7. Are the omicron variants less dangerous than the others we have seen?
The omicron variants appear to produce less severe illness in adults and more serious cases in children when compared to the delta variant. That was based upon South Africa’s experience, which showed a 50% decrease in hospitalizations per 100,00 infected people.
So far, people in England have been 40–45% less likely to require hospitalization for omicron than for the delta variant; they are 20% less likely to seek emergency services at the hospital.
The newer BA.2 subvariant produces illness of the same severity as the original omicron variant.
After accounting for prior infection and vaccination status in a region of California with a mixture of delta and omicron cases, researchers compared the severity of infection of the two variants. In comparison to people infected with the delta variant, those with omicron:
- Were 53% less likely to need hospital care
- If hospitalized, had a 70% shorter stay
- Had a 74% lower ICU admission rate if hospitalized
- Experienced a 91% decrease in deaths
Per 1,000 cases of Covid due to the omicron variant by January 15, 2022, in the US:
- 27 were admitted to the hospital for an average stay of 5.5 days
- 3.5% needed a ventilator
- 9 died (there is a three-week lag after diagnosis)
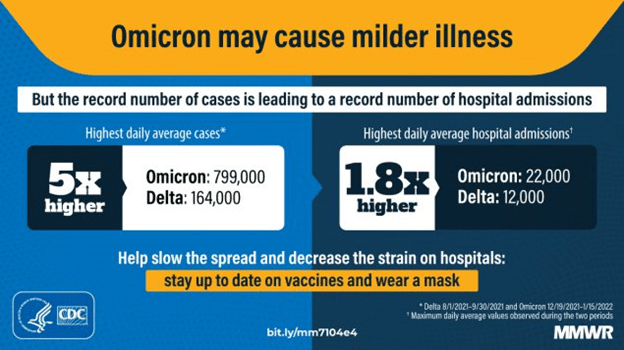
However, omicron (R0 = 10 for B.1.1259; R0 = 13 for the newer BA.2) spreads much more easily than the delta variant (R0 = 7). That means the average person with the omicron variant will infect ten or thirteen people, versus seven for delta.
Even if the likelihood of hospital admission is half that of delta, much like compound interest in banking, that increased transmissibility means a much higher rise in Covid hospitalizations.
The Inside Medicine: Omicron Paradox link has a fantastic visualization of this phenomenon. It is happening at a time when many health care workers are in quarantine after testing positive.
Approximately one-third of official admissions are due to a primary Covid diagnosis; one-third are due to Covid making an underlying condition worse; and one-third are admitted for another reason. In-patients tend to have shorter stays and are less likely to require an ICU bed than with the delta variant, dropping from roughly 25% to 10%.
Here is what happened in Florida. A 31% positivity rate means there were likely five undiagnosed infections for each new positive test. The two charts on top are for the week beginning on February 18, 2022:



Eighty percent of Covid admissions at Tampa General Hospital are for people who have not received a primary vaccination series.
Someone I know died during the first week of January after five days in the hospital on a ventilator, so it’s not something to take lightly. Less severe than delta can still be deadly.
MedPage: No Real-World Evidence BA.2 Is More Severe
MRC Centre: Report 50 – Hospitalisation Risk for Omicron Cases in England
Inside Medicine: The Omicron Paradox: If It’s Milder, Why Are Hospitals on the Brink of Disaster?
Tampa Bay Times: Florida COVID Hospital Admissions Highest Since Summer as Omicron Spreads
Feb 25, 2022 Florida Covid Stats: What Is Really Happening?
Salemi USF: COVID-19 in Florida Hospital Admissions by Age
.
.
8. With other variants, older people and those in poor health were most likely to have a severe case or die. Is that still true with the omicron variant?
In a part of California with a mixture of Covid cases due to the delta variant and the omicron variant, the highest hospitalization rates for those with omicron occurred in people aged 20–39. They were less likely to have comorbidities than individuals who needed hospital care for the delta variant.
A study in Sweden determined that unvaccinated elderly people and middle-aged males with comorbidities are most likely to experience severe disease from the omicron variant:

The CDC maintains a full list of comorbidities here.
Among adults under 60, the demographic groups with the largest rates of increase in severe Covid cases in Florida correspond to the percentage of people vaccinated within that age group. Vaccination makes an enormous difference:

| Age | % Change Admissions |
| 0–17 | 218 |
| 18–29 | 367 |
| 30–39 | 184 |
| 40–49 | 157 |
| 50–59 | 92 |
| 60–69 | 96 |
| 70+ | 118 |
| all ages | 140 |

Here is what one doctor who treats Covid patients in NYC has testified:
- People who have received a booster shot are likely to experience symptoms like those of a mild common cold
- Those with two doses of an mRNA vaccine tend to feel sicker than those with booster shots but can still breathe
- Individuals with one dose of Johnson & Johnson often feel miserable, with some shortness of breath but do not require oxygen or hospitalization
- Unvaccinated people are 15 times more likely to need hospital care for extreme shortness of breath requiring oxygen
CDC: People with Certain Medical Conditions
Salemi USF: COVID-19 in Florida
CDC: Omicron Variant: What You Need to Know
4 New York: NYC ER Doc Breaks Down How Omicron Affects the Boosted, Vaxxed, and Unvaccinated
.
.
9. What pre-exposure options are available for people who don’t develop an immune response to vaccines, like transplant patients or individuals with some blood cancers?
On December 8,2021, the FDA issued an Emergency use Authorization for Evusheld, a monoclonal antibody developed for people over the age of 12 with severe immunosuppression. The National Infusion Center maintains a web site listing facilities which can deliver this preventative treatment.
Evusheld appears to remain effective against the omicron BA.2 subvariant. However, due to that subvariant, the FDA amended the EUA on February 24, 2022, to double the dosage of each component of Evusheld.
People who had already received it should contact their physicians about an additional shot. The FDA is now uncertain how long the immunity conferred by Evusheld will last.
FDA: FDA Authorizes Revisions to Evusheld Dosing
.
.
10. I have been exposed to SARS-CoV-2 or tested positive in the last 5–10 days. Are there safe and effective treatments available?
Monoclonal antibodies are made in a lab to mimic those which occur naturally after infection with SARS-CoV-2. People over the age of twelve who are at high risk of severe illness are eligible to receive that treatment at no cost. Unfortunately, there are going to be severe supply issues.
For the delta variant, an infusion given after exposure or when symptoms were still mild was 70% effective at preventing hospitalization or death.
Mutations which have resulted in the omicron variant render ineffective almost all the monoclonal antibodies currently in use.
The antibody combination used in Regeneron against the delta variant (imdevimab and casirivimab) fails to inhibit omicron.
There are only one or two monoclonal antibodies produced in the US and UK which can attach to circulating omicron particles.
Sotrovimab, known commercially as Xevudy, works against the original omicron variant at a dosage three times that required to neutralize the delta variant.
Unfortunately, Sotrovimab fails to adequately neutralize the omicron BA.2 subvariant. The only monoclonal antibody in production which works against all omicron variations is a new one called bebtelovimab.
.
.
With the sudden shift in predominating strains, it is likely to be very difficult even for people at the highest risk to access the limited supply of monoclonal antibody treatment for an omicron infection. If you have been relying on that option, this is a great time to get vaccinated instead.
Due to the overwhelming demand for this medication, the NIH has released updated guidelines prioritizing monoclonal antibody treatment for those at the highest risk of progressing to severe Covid-19: people who test positive and are unvaccinated or are unlikely to develop a sufficient antibody response after vaccination and fall into at least one of these categories:
an age of at least 65 years; has cancer, cardiovascular disease, diabetes, chronic kidney, or lung issues; has a compromised immune system or is taking immunosuppressive medication; has a body mass index over 30; is pregnant; or has sickle cell disease. Those with multiple comorbidities receive the highest priority.
You can click here for additional information if you suspect you are infected with either variant.
Receiving monoclonal antibodies is likely to increase your susceptibility to reinfection.
The current recommendation for monoclonal antibody recipients regarding any Covid vaccination is to wait for 90 days after the infusion or injection to prevent the treatment from interfering with your immune system’s ability to produce antibodies.
.
.
On December 22, 2021, the FDA approved an oral antiviral treatment for adults and children with mild-to moderate illness who fall into the categories eligible for monoclonal antibodies. Clinical trials showed Paxlovid is 90% effective at preventing hospitalization and death. Ingestion of this prescription medication must begin within five days of the first symptoms.
Paxlovid is not authorized as a substitute for vaccines, nor can it be prescribed to prevent Covid. Production takes 6–8 months, so this medication will also be extremely hard to access despite the US government’s order of doses for ten million Covid patients.
Another oral medication (Molnupiravir) approved for treating the omicron variant is far less effective. It decreased the risk of hospitalization or death by about one-third.
Data for the weekly allocation of Covid-specific treatments to each state is available at this link: State/Territory-Coordinated Distribution of COVID-19 Therapeutics
Use of the older intravenous treatment Remdesevir has been expanded to outpatients over a three-day course. Against omicron, it remains 87% effective at preventing hospitalization or death. Early in the pandemic, this medication fell out of favor due to the high adverse reaction rate (55%).
NEJM: REGEN-COV Antibody Combination and Outcomes in Outpatients with Covid-19
NEJM: Efficacy of Antibodies and Antiviral Drugs Against Covid-19 Omicron Variant
Pharm Tech: GSK’s Sotrovimab Retains Activity Against Omicron Variant
NIH: Updated COVID–19 Treatment Guidelines Panel‘s Statement on the Prioritization of Anti-SARS-CoV-2 Monoclonal Antibodies for the Treatment of Prevention of SARS-CoV-2 Infection When There Are Logistical or Supply Constraints
Allergy & Asthma Network: What Is Monoclonal Antibody Infusion Therapy for COVID-19
Nature: Antibody Evasion Properties of SARS-CoV-2 Omicron Sublineages
CDC: Interim Clinical Considerations for Use of COVID-19 Vaccines Currently Approved of Authorized in the United States
NEJM: Molnupiravir for Oral Treatment of Covid-19 in Nonhospitalized Patients
NEJM: Early Remdesevir to Prevent Progression to Severe Covid-19 in Outpatients
Frontiers in Med: Mortality Benefit of Remdesevir in COVID-19: A Systematic Review and Meta-Analysis
.
11. Can people who were previously infected get Covid again? How does natural immunity compare to the immunity from vaccines? Do monoclonal antibodies increase the risk of reinfection?
Here is what we know so far about the percentage of people whose blood samples showed sufficient antibody protection. Note that booster efficacy will decline another 15–20% after 10 weeks:
- Had the delta variant, not vaccinated = 15%
- Had the alpha variant, not vaccinated = 10%
- Recovered from Covid + AstraZeneca vaccine = 100%
- Recovered from Covid + Pfizer vaccine = 100%
- Two doses of the AstraZeneca vaccine = 0%
- One dose of the Johnson & Johnson vaccine = 8%
- Two doses of the Pfizer vaccine = 30–45%
- Two doses of the Moderna vaccine = 50%
- Three doses AstraZeneca = 67%
- Two doses AstraZeneca + one dose Pfizer = 71%
- Three doses Pfizer = 76%
- Three doses Moderna = 88%

In England, a population-based study revealed that those with a prior Covid infection were five times more likely to become infected with omicron compared to reinfection with other variants. The researchers estimate that only one-fifth of unvaccinated people who previously tested positive can fend off the omicron variant.
People who have received monoclonal antibodies for a previous Covid infection are more likely to become reinfected.
Lancet: Omicron Variant and Booster Covid-19 Vaccines
MedRxiv: Broadly Neutralizing Antibodies Overcome SARS-CoV-2 Omicron Antigenic Shift
Imperial College: Omicron Largely Evades Immunity from Past Infection or Two Vaccine Doses
MedPage: Early UK Data: Two Vax Doses Don’t Cut It Against Omicron—But Booster Bumps Effectiveness to More than 70%, Technical Briefing Finds
MedRxiv: Booster of mRNA-1273 Vaccine Reduces SARS-CoV-2 Omicron Escape from Neutralizing Antibodies
MedRxiv: Omicron-B.1.1.529 Leads to Widespread Escape from Neutralizing Antibodies
MedRxiv: Effectiveness of COVID-19 Vaccines Against the Omicron (B.1.1.529) Variant of Concern
Allergy & Asthma Network: What Is Monoclonal Antibody Infusion Therapy for COVID-19
.
.
12. Why do the vaccines decrease the risk of hospitalization or death? How effective are they?
In serious cases, people have the fever and cough for several days before breathing problems develop. The virus shuts down the part of their immune systems which produce neutralizing antibodies. Instead, their immune systems create a non-neutralizing form of IgG antibody which causes severe inflammation. A “cytokine storm” then damages the lungs, heart, liver, kidneys, and brain.
In contrast, vaccination-induced immunity is characterized by the production of IgG antibodies which neutralize the virus while reducing inflammation.
.
An early study regarding Vaccine Effectiveness in the UK compared adults over the age of 65 who received an mRNA booster shot to people in that demographic group who did not. For the first 2–9 weeks, boosted individuals were 50% less likely to have a symptomatic infection from the omicron variant. That percentage dropped to 25% after 10 weeks.
Six months after receiving two doses of any Covid vaccine in the UK, adults over 49 years old were 60% less likely to die due to the omicron variant.
Any combination of a primary two dose vaccine series followed by a Pfizer booster prevented 90% of hospitalizations during the first 2–9 weeks. During the 10 though 14th week, that Vaccine Effectiveness fell to 75%.
A Moderna booster is 90–95% protective against hospitalization for the first 9 weeks. Follow-up data for that vaccine is not yet available.
Taking a snapshot on December 25, 2021—the most recent date for available data—unvaccinated adults in the US were 18 times more likely to require hospital care for Covid than adults who had completed a vaccination series (78.2/100,000 vs. 4.3/100,000). Overall, Vaccine Effectiveness at preventing hospitalization was 94%:

For adults aged 50–64 during December 19–25, the CDC has added people who received booster shots as a separate category.
Unvaccinated people in this age group at a rate of 72/100,000. Those who finished a vaccine series had 87% fewer hospitalizations than expected. A booster dose prevented 97% of hospitalizations:

Results for that same week for senior citizens showed that unvaccinated individuals required hospital care at a rate of 239.7/100,000.
Completing a vaccine series reduced the likelihood of needing hospitalization by 89%. Adding a booster prevented 98% of hospitalizations which would have occurred without vaccination:

Among immunocompromised people in the US during the delta wave, those who had a third dose of an MRNA vaccine experienced 88% fewer hospitalizations than unvaccinated people with compromised immune systems. Two doses provided protection to 69% of them. The study team expects a similar degree of improvement with a third dose vs. two shots against the omicron variant.
UK residents who received any mRNA booster shot saw their risk of death drop by 90% compared to their unvaccinated peers. As of late January 2022, 80% of adults in the UK had received booster shots.
.
Last summer in the UK, 90% of adults had received at least one dose of a vaccine. That decreased the risk of hospitalization by 96%. However, slightly more than half of deaths occurred in fully vaccinated people.
Compare an 80-year-old fully vaccinated man with a 45-year-old unvaccinated man. The risk of death from Covid doubles with every seven years of age. Dropping the likelihood of death 20 times by being vaccinated cannot offset increasing the risk of being 80 years old by 32 times.
The Lancet: COVID-19: Consider Cytokine Storm Syndromes and Immunosuppression
UK Health Security: Boosters Provide High Level of Protection Against Death with Omicron
CDC: Rates of Laboratory-Confirmed COVID-19 Hospitalizations by Vaccination Status
.
13. How risky is post-vaccination myocarditis for younger people? How does the risk of other vaccine side effects compare to the symptoms of Covid?
Concerns about myocarditis and pericarditis after vaccination have prevented many young men and women from getting vaccinated. For the mRNA vaccines, they have occurred at a rate of 12.6/million. People who experience this side effect have chest pain within 2–3 days after receiving their second dose of an mRNA vaccine. Almost all cases remained mild, and the patients fully recovered.
In contrast to the myocarditis arising from vaccination, the inflammation resulting from SARS-CoV-2 can cause life-threatening heart conditions in children, adolescents, and adults:

Research into 2.4 million vaccine recipients, who were equally divided between the Moderna and Pfizer vaccine, identified fifteen men between the ages of 18 and 40 who required hospitalization for myocarditis. All responded well to standard treatment. There was no statistical difference between Moderna and Pfizer recipients (seven vs. eight).
During December 19–25, 2021, fully-vaccinated adolescents required hospitalization 92% less often than their unvaccinated peers (5.9/100,000 vs. 0.5/100,000):

With the omicron variant transmitting more easily than chickenpox, it is far safer to get vaccinated.
On October 29, 2021, the FDA approved Pfizer vaccine’s Emergency Use Authorization in children 5–11 years old. It prevented 90% of SARS-CoV2 infections. Among the 3,100 children who received the vaccine during clinical trials, there were no cases of myocarditis, pericarditis, anaphylaxis, or death. Children who experienced fatigue, muscle pain, or headache after vaccination recovered within two days.
MedRxiv: Risk of Myocarditis from COVID-19 Infection in People Under Age 20: A Population-Based Analysis
Circulation: Myocarditis with COVID-19 mRNA Vaccines
JAMA: Acute Myocarditis Following COVID-19 mRNA Vaccination in Adults Aged 18 Years or Older
CDC: Rates of Laboratory-Confirmed COVID-19 Hospitalizations by Vaccination Status
.
A study of two million people in Israel compared the likelihood of experiencing a significant Pfizer vaccine-induced side effect to the risk of those same symptoms of Covid-19. Here are the results:

Compared to those infected with SARS-CoV-2, people vaccinated with two doses of the Pfizer vaccine were substantially protected against acute kidney injury, cardiac arrythmia, deep vein thrombosis, hemorrhagic stroke, heart attack, myocarditis, inflammation surrounding the heart, blood clots in the lung, erectile dysfunction, and reduced male fertility.
While cases of shingles remained rare among individuals in that study, there was an increase in risk among those who received the vaccine.
The Radiological Society of North America recommends waiting 4–6 weeks after the final dose of an mRNA vaccine to undergo a routine mammogram, noting that swelling of lymph nodes in the armpit (lymphadenopathy) is a normal immune response that resolves with time.
This is a side effect which I experienced. While I was aware of a lump for a few weeks, it didn’t cause any problems. Nevertheless, I did mention it to the woman who did my mammogram. She then asked which arms had received the injections in case any swelling appeared in the scans.
NEJM: Safety of the BNT162b2 mRNA Covid-19 Vaccine in a Nationwide Setting
JAMA: Sperm Parameters Before and After COVID-19 mRNA Vaccination
The Conversation: COVID-19 Could Cause Male Infertility and Sexual Dysfunction—but Vaccines Do Not
RSNA: Covid-19 Vaccine-Related Lymphadenopathy: What to Be Aware Of
.
14. Are mRNA vaccines safe for pregnant women and their babies?
Research comparing miscarriages, preterm births, and low birth weights as pregnancy outcomes for vaccinated women and women who were pregnant before the pandemic found no differences between them. No neonatal deaths occurred among vaccinated women.
Newborns whose mothers were vaccinated early in the third trimester produced a greater antibody response compared to those whose mothers received a vaccine closer to the time of delivery.
Vaccinated women who breastfed their infants secreted Covid-specific antibodies in their milk for at least six weeks. That provided protection to their newborns.
Milk from breastfeeding women who received either mRNA vaccine did not yield any detectable vaccine in the days after vaccination.
On the other hand, pregnant women who become infected with SARS-CoV-2 are more likely to experience severe illness requiring hospitalization, breathing assistance, or ventilation. They also have increased risk of preterm delivery or death.
From March 2020–October 2021, fifteen pregnant women died from Covid in in Mississippi alone. Almost all had underlying conditions and most died a few days after giving birth. None were fully vaccinated. The delta variant increased the likelihood of death five times compared to the original SARS-CoV-2 virus, from five deaths/1,000 pregnant women with Covid-19 to 25/1,000. During the time when the delta variant predominated, pregnant women infected with SARS-CoV-2 in Mississippi were eight times more likely to die than infected women of similar ages who were not expecting a child. Black and Hispanic women were at greatest risk.
A study of 1,250,000 births in the US from March 2020 through September 2021 found that pregnant women infected with the delta variant are four times as likely to experience stillbirth as uninfected women. Investigators in this study were not able to assess their vaccination status. As of July 2021, only 30% of pregnant women were fully vaccinated.
That is why the American College of Obstetrics and Gynecology enthusiastically recommends that all pregnant women receive vaccination and Pfizer booster shots, and the CDC has issued an urgent advisory.
Similar results occur with the AstraZeneca vaccine, and a second dose is recommended for women who become pregnant after starting the series. However, due to more research on pregnancy with the mRNA vaccines, Pfizer or Moderna are preferable for unvaccinated women.
NEJM: Preliminary Finding of mRNA Covid-19 Vaccine Safety in Pregnant Persons
NEJM: Receipt of mRNA Vaccines and Risk of Spontaneous Abortion
JAMA: Spontaneous Abortion Following COVID-19 Vaccination During Pr
JAMA: Evaluation of Messenger RNA from COVID-19 BTN162b2 and mRNA-1273 Vaccines in Human Milk
CDC: COVID-19 Vaccines While Pregnant or Breastfeeding
ACOG: COVID-19 Vaccination Considerations for Obstetric–Gynecologic Care
Royal College of Obstetricians and Gynaecologists: Covid-19 Vaccines, Pregnancy, and Breastfeeding
.
15. What about the risk of infertility?
Women may experience irregular menstrual cycles or changes in flow after vaccination or after having Covid-19. This is common for infections and immune system reactions and lasts for only a few months. The North American Society for Pediatric and Adolescent Gynecology recommends vaccination for adolescents and young adults.
In a large fertility study, women who were vaccinated were slightly more likely to become pregnant. Getting Covid had no effect upon the fertility of women in the study. However, when their male partners became infected, they experienced an 80% reduction in the likelihood of conception during the first month. After 60 days, their fertility was restored.
A recent study confirmed that antibodies to the SARS-CoV-2 spike protein have no effect upon the implantation of an embryo or pregnancy development. In women, neither natural infection nor vaccination cause sterility.
Receiving an mRNA Covid vaccine did not affect ovarian stimulation or early pregnancy outcomes among women using In Vitro Fertilization.
Another study involving sperm counts in men found that sperm concentration and motility increased after the second vaccination. In contrast, research on men who contracted Covid-19 found reduced fertility and erectile dysfunction.
ASRM: New Study Reveals Covid Vaccine Does Not Cause Female Sterility
Royal College of Obstetricians and Gynaecologists: Covid-19 Vaccines, Pregnancy, and Breastfeeding
JAMA: Sperm Parameters Before and After COVID-19 mRNA Vaccination
The Conversation: COVID-19 Could Cause Male Infertility and Sexual Dysfunction—but Vaccines Do Not
.
16. How can I discuss this with people I love who are vaccine-hesitant?
Here is an explanation I gave to a friend who had been terrified about getting vaccinated until a mutual friend got Covid:
The day of our friend’s diagnosis, she got vaccinated but called me the next day because she wasn’t feeling great. I explained the vaccine to my friend using coral snakes and milk snakes to illustrate:
“Your immune system is encountering what it thinks is a coral snake and is rising up to kill it. If you’re not feeling good, it’s because your immune system is working to destroy a coral snake. Since there’s no genetic material there, it can’t reproduce, and it does not affect your DNA. Within a few days your liver clears out what’s left.
“Right now, you’re 30% protected from the delta variant. When another milk snake comes along, your immune system produces more protection to destroy what looks like the same threat.
“Two weeks after the second dose, when your immune system sees a coral snake, it’s prepared to overwhelm it before it can make you very sick. Based on what I’m seeing, most of the antibodies are in lymph nodes in your chest. That explains why fully vaccinated people who do get infected usually have mild cold symptoms. The virus gets neutralized before reaching your lungs.”


MedLine Plus: What are mRNA Vaccines and How Do They Work?
Ad Drug Deliv Rev: Controlling Timing and Location in Vaccines
UAB: Three Things to Know about the Long-Term Side Effects of COVID Vaccines
.
17. What sources can I trust?
1) Health Data.Gov – COVID-19 Community Profile Report – Updated every weekday
2) World Health Organization Situation Reports – These tend to be one day behind. Some nations are not keeping their information up to date: WHO: Situation Reports
3) Johns Hopkins University – Johns Hopkins Univ: Coronavirus Resource Center – Not recommended for Florida statistics as that state updates only once per week, is hiding deaths, and does not include any non-resident data.
4) MedPage Today – MedPage Today: Covid -19 Updates
5) Investigation of SARS-CoV-2 Variants of Concern: Technical Briefings – for the UK
6) Redemptive History and Theology – Covid-19 Information covers broader Covid-19 issues, including medical and theological perspectives
7) HHS Protect Public Data Hub – Hospital Utilization by facility or by state
8) CDC: Covid-19 Integrated County View – transmission, cases, test positivity, deaths, hospital usage, % of vaccinated people, and a Social Vulnerability Index by county
9) Florida Statistics: What is Really Happening? – A review of Florida statistics showing what that state is trying to hide and how you can find the missing information.
10) Dr. Jason Salemi – Covid-19 Dashboard: A Focus on FL with National Comparisons
11) CDC: COVID-19 Community Levels
