This post is archived.
It addresses issues specifically concerning the delta variant. You can access my most recent post here.
.
1. How Was the US Managing Covid-19 Until Recently?
2. Does the delta variant have different symptoms from previous SARS-CoV-2 variants? Are vaccinated people who get infected contagious?
3. How does a virus variant arise?
4. When and where did the delta variant originate?
5. How fast has the delta variant spread in the US? What percentage of cases occurring now are caused by that variant?
6. What is an R0 number in disease transmission? How has it changed from other SARS-CoV-2 variants? Why are vaccinated people getting breakthrough infections? Is natural immunity better?
7. Is the delta variant more dangerous than the others we have seen?
8. With other variants, older people and those in poor health were most likely to have a severe case or die. Is that still true with the delta variant?
9. I have been exposed to SARS-CoV-2 or tested positive in the last ten days. Is there a safe and effective treatment available? How can I access it?
10. Can people who were previously infected get Covid again? How does natural immunity compare to the immunity from vaccines?
11. How well does one dose of a vaccine protect me from the delta variant compared to full vaccination?
12. How long does the protection from an mRNA vaccine last? Why are booster shots being recommended, and who should get one? If I got the Johnson & Johnson vaccine, should I get an mRNA booster?
13. How effectively do the vaccines protect us from hospitalization or death?
14. How risky is post-vaccination myocarditis for younger people? How does the risk of other vaccine side effects compare to the symptoms of Covid?
15. Are mRNA vaccines safe for pregnant women and their babies?
16. What about the risk of infertility?
17. How can I discuss this with people I love who are vaccine-hesitant?
18. What sources can I trust?
.
About me: I have a masters’ degree in Infectious Disease Epidemiology from UCLA, a bachelors’ degree from Wheaton College in biology with a certificate in International Community Development, and a masters’ in Greek and Hebrew Exegesis from Gordon-Conwell Theological Seminary. Usually, I am writing and posting bible studies on the Redemptive History Facebook page, but these are not normal times.
I began my career by editing a medical monograph and writing an accompanying peer-reviewed journal article during my graduate studies at UCLA (MPH, Tropical and Infectious Disease Epidemiology). My first publication concerned the excess risk of severe illness or death from a bacterium in raw milk in California. It was featured on the front page of the Los Angeles Times and was debated in the state legislature.
After graduation, I conducted records-based research concerning the efficacy of a poly-pharmacy reduction program for nursing home residents. We focused upon the frequency and severity of adverse drug reactions, and whether our patients could stop taking their medications without needing to resume using them. Textbooks still cite it today.
Paul Terrill MD, FAAFP has been an invaluable collaborator in assessing and compiling many of these resources.
.
Due to the sudden onset and severity of the pandemic, many journals are pre-empting their normal four-week to six-month process of peer reviewing articles before releasing them for publication. When you look at any research involving Covid-19, it is important to note the status of the article: pre-print or accepted for publication after peer review. Check the comments under pre-print articles. Several major studies were retracted after the peer-review process detected significant issues.
Lancet, NEJM retract studies on hydroxychloroquine for COVID-19
.
1. How Was the US Managing Covid-19 Until Recently?
Only a few weeks ago, in early July 2021, infectious disease experts were feeling hopeful. As more people received full immunization, Covid-19 cases were diminishing. Reaching herd immunity soon seemed possible. Virtually all Covid-19 cases, hospitalizations, and deaths were occurring in unvaccinated people:
- For every 147 positive tests, one person was vaccinated
- For every 259 hospital admissions, one person was vaccinated
- For every 167 deaths, one person was vaccinated

To see how I calculated the information in this graphic, you can click here: https://redemptivehistorytheology.com/wp-content/uploads/2021/07/jan-1-to-apr-30-covid-stats.pdf
Emerging information about the delta variant is rapidly changing how we respond.
.
2. Does the delta variant have different symptoms from previous SARS-CoV-2 variants? Are vaccinated people who get infected contagious?
People infected with the delta variant are less likely to experience cough or the loss of smell. The loss of smell usually accompanies a milder infection, so this does fit with the increased virulence we are now seeing. Delta variant infections often produce a headache, runny nose, sore throat, congestion, sneezing, muscle pain, and fever.
To see a full listing of Covid-19 symptoms, click here.
.
Symptoms which require immediate emergency medical care include difficulty breathing, continuous pressure or pain in the chest, an inability to awaken or to stay awake, a new onset of confusion, or a blue tinge in the face or lips.
Investing in a pulse oximeter to track your blood oxygen level is a great idea. They cost about $20. A normal oxygen saturation level runs between 95–100%. People with Covid-19 can experience a drop in that percentage without realizing it has happened. If it does occur, seek medical attention immediately.
Fully vaccinated people who get infected often have symptoms of a mild cold. They can still spread the virus just as easily as unvaccinated people.
That is why the CDC now recommends everyone wear a mask in indoor public spaces in localities with high rates of transmission.
Yale Medicine: Five Things to Know about the Delta Variant
CDC: Interim Public Health Recommendations for Fully Vaccinated People
.
3. How does a virus variant arise?
Random mutations occur due to errors in the viral replication process. While coronaviruses have an enzyme which corrects most of those mistakes, some do still slip through to create a new variant.
Only those mutations which confer an advantage to viral replication, transmission, or survival of immune systems expand in a host population. Since mutations are random, vaccine developers cannot predict in advance what a virus will look like in the future.
JAMA: Genetic Variants of SARS-CoV-2—What Do They Mean?
.
4. When and where did the delta variant originate?
Originally called B.1.617.2, the delta variant was initially identified in India in December 2020. It appears to have arrived in the US in March 2021, when the nation’s mass vaccination program was well underway. Mayo Clinic maintains a list of the variants of greatest concern world-wide.
CDC: About Variants of the Virus that Causes COVID-19
Mayo: COVID-19 Variants: What’s the Concern?
.
5. How fast has the delta variant spread in the US? What percentage of cases occurring now are caused by that variant?
On April 24, 2021, the delta variant accounted for 0.6% of the SARS-CoV-2 genetically sequenced specimens in the US. During August 14–December 4, 2021, it accounted for 98–99% of Covid cases. On December 11th, the omnicron variant was detected in 3% of sequenced samples in the US, a 700% increase over two weeks. The CDC’s interactive dashboard shows the proportion of each variant over time for the US as a whole and for each region. It is currently updated every two weeks.
.
6. What is an R0 number in disease transmission? How has it changed from other SARS-CoV-2 variants? Why are vaccinated people getting breakthrough infections? Is natural immunity better?
An R0 (“R naught”) represents the basic reproduction rate of a pathogen: how many people become infected when exposed to a single case. When an R0 is larger than 1.0, an outbreak is increasing; when it is less than 1.0, an epidemic is waning. Human behavior and the properties of an infectious agent both impact disease transmission, so some variability does exist.
Researchers use the R0 to estimate the proportion of a population that must no longer be susceptible to infection to reach herd immunity. That can typically be achieved by a combination of surviving natural infection and immunization.
Diseases with a higher R0 require more people with immunity for transmission to stop.
CDC Emerg Inf Dis: Complexity of the Basic Reproduction Number (R0)
.
The original strain of the virus which came from China had an R0 of 2.5; in the UK, the delta variant is almost three times more transmissible with an R0 of approximately 7.
However, on July 29, 2021, the CDC estimated the delta variant is just as transmissible as chickenpox. Chickenpox has an R0 of 9–10, which means that the average person with that virus infects 9 or 10 people. As a result, 89–90% of the population surrounding an infected individual must be immune to prevent spreading that disease.
For those of us too old to have received the vaccine to prevent chickenpox, how many of us escaped infection?
That is why many experts are warning that anyone unvaccinated against Covid-19 in the US will almost certainly contract the infection. Please do not make the mistake of equating transmissibility with severity. Covid-19 is far more dangerous than chickenpox.
Lancet: Lifting of COVID Restrictions in the UK and the Delta Variant
JHU: Measuring Disease Dynamics in Populations: Characterizing the Likelihood of Control
.
In August 2021, unvaccinated people were 6 times more likely to test positive for the virus that causes Covid-19 than fully vaccinated individuals.
Compared to the original strain of SARS-CoV-2, even vaccinated people infected with the delta variant carry 250 times the amount of virus.
Two weeks after vaccination, the antibody level of saliva from people vaccinated with either mRNA vaccine is comparable to that of people who have recovered from Covid.
That does not include the one-third of people who tested positive for SARS-CoV-2 and were sick who showed no antibody response three weeks after they felt better. Some of them were severely ill. This happened most often in younger adults.
After several months, a comparison of antibody levels in Moderna and Pfizer recipients revealed over twice the number of antibodies produced by the Moderna vaccine. This is likely due to the increased amount of mRNA in Moderna and the longer interval between doses.
Following vaccination or natural infection, when we are exposed to the virus, our circulating antibodies attach to the spike protein of SARS-CoV-2, preventing the virus from entering a cell. When there are more viral particles than available antibodies, the virus breaks through our defenses. How we behave has an enormous impact on the amount of virus we encounter.
Once inside, the delta variant reproduces so rapidly that it can spread before our immune system has time to react, enabling the virus to spread to others. However, the vaccines also produce T cell immunity. Our T cells go on a search and destroy mission, killing any infected cells and neutralizing the virus within them. This significantly shortens how long vaccinated people can spread the virus.
People who are fully vaccinated produce more antibodies and a much stronger T cell response than those infected with SARS-CoV-2 one year ago.
In addition to people carrying a greater amount of the delta variant of the virus, one study found that people with the delta variant shed it for an average of eighteen days vs. thirteen days for other variants. That may also be why the R0 is higher.
Three-fourths of transmission is occurring during the two-day window before symptoms develop, Days 4–6 after exposure to SARS-CoV-2. Compared to people who are unvaccinated, fully vaccinated people are two-thirds less likely to spread the virus to others.
This analogy by Dr. Leana Wen is helpful: “Think of the vaccine as a very good raincoat. It keeps you dry in a drizzle. If there are constant thunderstorms, you may get wet. The problem isn’t the raincoat—it’s the weather. To best protect all of us, we need to reduce the storm of Covid-19 by increasing vaccination rates.”
CDC: Rates of COVID-19 Cases and Deaths by Vaccination Status
Emerg Inf Dis: Predictors of Nonseroconversion after SARS-CoV-2 Infection
JAMA: Comparison of SARS-CoV-2 Antibody Response Following Vaccination with BNT162b2 and mRNA-1273
.
7. Is the delta variant more dangerous than the others we have seen?
Unfortunately, the delta variant is causing significantly more severe illness and death than the other variants we have seen so far during this pandemic.
In one study, patients with the delta variant were 88% more likely to develop pneumonia compared to those with other strains of SARS-CoV-2.
Other researchers found that people infected with the delta variant were hospitalized 85% more often than for other variants, even when matched with patients of the same age, sex, socioeconomic status, and comorbidities.
A preprint study conducted in Canada determined that people with the delta variant were 120% more likely to require hospitalization, needed care in the ICU 287% more often, and died 137% more often than people who contracted other variants.
MedRXiv: Progressive Increase in Virulence of Novel SARS-CoV-2 Variants in Ontario, Canada
.
In the US overall, hospital admission for Covid-19 for the week of August 11–17, 2021 increased by 14.2% over the previous week.
Florida reported a record 10,207 hospitalizations for Covid-19 on August 1, 2021 to the US Department of Health and Human Services. On August 20th, that number increased by 69% to 17,235, with 3,585 Covid patients in ICU beds.
Tampa General Hospital’s Covid patients more than doubled from 113 to 246 during August 1–20; its ICU had less than 10% availability during that entire period, rising from 51 to 103 people.
CDC Covid Data Tracker Weekly Review: Interpretive Summary for July 30, 2021
Florida Statistics: What is Really Happening?
HHS Protect Data Hub: Hospital Utilization
Tampa General Hospital: Hospital Bed Availability for COVID-19 Patients
.
8. With other variants, older people and those in poor health were most likely to have a severe case or die. Is that still true with the delta variant?
According to the president of the Florida Hospital Association, this wave of Covid-19 due to the delta variant is dramatically different from what we previously experienced.
On August 2nd, Mary Mayhew stated, “In one of our hospitals, their average age now is 42 years old. They have 25-year-olds who are in intensive care, on ventilators…You have over 50% of our hospitalizations are between the ages of 25 and 55. It is a rapid increase, not only in hospitalizations, but in the deterioration. Sicker, sicker individuals. Again, pregnant women in our intensive care units. This is just dramatically different from what we saw last year… this is clearly ripping through the unvaccinated.”
She added that 96% of hospitalized Covid patients in Florida are unvaccinated and that younger people can no longer assume they are not at risk.
In Israel, a nationwide study found that no adolescents who received two doses of the Pfizer vaccine needed hospitalization for the Covid-19 delta variant, in contrast to one in every 300 of their unvaccinated peers.
A large study in the US revealed that over one-third of people who tested positive for SARS-CoV-2 continued to experience at least one symptom three to six months after being diagnosed.
After 22 pregnant women with Covid died in one month, the CDC issued an urgent health advisory stressing the need for vaccination on September 27, 2021. Ninety-seven percent of hospitalized pregnant women who tested positive for SARS-CoV-2 were unvaccinated.
From March 2020–October 2021, fifteen pregnant women died from Covid in in Mississippi alone. Almost all had underlying conditions and most died a few days after giving birth. None were fully vaccinated.
The delta variant increased the likelihood of death five times compared to the original SARS-CoV-2 virus, from five deaths/1,000 pregnant women with Covid-19 to 25/1,000. During the time when the delta variant predominated, pregnant women infected with SARS-CoV-2 in Mississippi were eight times more likely to die than infected women of similar ages who were not expecting a child.
As of August 12th, the American Academy of Pediatrics (AAP) noted that severe cases of Covid-19 remain uncommon among children. However, whether due to more efficient transmission or increased severity of the delta variant, many more children are being hospitalized for Covid.
Due to concerns about long-term physical and mental health effects, the AAP recommends continued monitoring of children who test positive.
During August through September 2021, Covid-19 was the number one cause of death among Americans aged 34–54. A sharp rise occurred in children as the delta variant gained hold.
Age-specific rank of COVID-19 deaths among leading causes of death in the US, 2021 as of October 6, 2021:
| Ages | Jan | Feb | Mar | Apr | May | Jun | Jul | Aug | Sep |
| 1-4 | 11 | 13 | 15 | 7 | 11 | 13 | 13 | 7 | 7 |
| 5-14 | 6 | 7 | 8 | 7 | 8 | 13 | 11 | 6 | 6 |
| 15-24 | 4 | 5 | 6 | 6 | 5 | 7 | 5 | 4 | 4 |
| 25-34 | 2 | 4 | 6 | 6 | 6 | 6 | 6 | 2 | 2 |
| 35-44 | 2 | 4 | 5 | 5 | 5 | 5 | 5 | 1 | 1 |
| 45-54 | 1 | 2 | 4 | 4 | 4 | 4 | 4 | 1 | 1 |
| 55-64 | 1 | 2 | 3 | 3 | 3 | 4 | 3 | 1 | 2 |
| 65-74 | 1 | 2 | 3 | 3 | 3 | 6 | 4 | 3 | 3 |
| 75-84 | 1 | 1 | 3 | 3 | 5 | 7 | 6 | 3 | 3 |
| 85+ | 1 | 2 | 5 | 5 | 6 | 8 | 7 | 3 | 3 |
| All ages | 1 | 1 | 3 | 3 | 3 | 6 | 8 | 3 | 2 |
AAP: Children and COVID-19: A State-Level Data Report
9. I have been exposed to SARS-CoV-2 or tested positive in the last ten days. Is there a safe and effective treatment available? How can I access it?
Monoclonal antibodies are made in a lab to mimic those which occur naturally after infection with the delta variant of SARS-CoV-2.
An infusion given after exposure or when symptoms are still mild is 70% effective at preventing hospitalization or death.
People over the age of twelve who are at high risk of severe illness are eligible to receive this treatment at no cost.
Due to the overwhelming demand for this medication, the NIH has released updated guidelines prioritizing monoclonal antibody treatment for those at the highest risk of progressing to severe Covid-19: people who test positive and are unvaccinated or are unlikely to develop a sufficient antibody response after vaccination and fall into at least one of these categories:
an age of at least 65 years; has cancer, cardiovascular disease, diabetes, chronic kidney, or lung issues; has a compromised immune system or is taking immunosuppressive medication; has a body mass index over 30; is pregnant; or has sickle cell disease. Those with multiple comorbidities receive the highest priority.
You can click here for additional information.
The current recommendation for monoclonal antibody recipients regarding any Covid vaccination is to wait for 90 days after the infusion or injection to prevent the treatment from interfering with your immune system’s ability to produce antibodies.
MedRxiv: REGEN-COV Antibody Cocktail Clinical Outcomes Study in Covid-19 Outpatients
CDC/IDSA: COVID-19 Clinician Call January 30, 2021
10. Can people who were previously infected get Covid again? How does natural immunity compare to the immunity from vaccines?
Natural immunity from prior infection to prevent acquiring the delta variant appears to last about six months in people who develop antibodies. Given the highly infectious nature of this variant, reinfection is likely to occur after that without vaccination.
How do we know this?
- The level of antibodies corresponds to the degree of protection against severe Covid
- One-third of people who tested positive for SARS-CoV-2 and were sick showed no antibody response three weeks after they felt better. Some of them were severely ill. This happened most often in younger adults.
- Less than half of people who recovered from Covid had detectable antibodies one year later
- Eighty percent of reinfections occur in people without full vaccination.
- Among people hospitalized for respiratory infections in the US, those with a previous SARS-CoV-2 infection at least three months before who remained unvaccinated were five times as likely to test positive for the virus when compared to people immunized with an mRNA vaccine who did not have a prior SARS-CoV-2 infection.
- Compared to people who were fully vaccinated, those who recovered from Covid had lower amounts of antibodies and a reduced T cell response one year after infection. The researchers strongly recommended that everyone with a natural infection get vaccinated.
In a study in Israel, people who recovered from Covid and received one dose of a vaccine cut their risk of reinfection in half.
People with Covid who want to become vaccinated should wait at least ten days after their symptoms first appears and 24 hours after their fever has broken and their other symptoms have subsided. That does not include the loss of taste or smell. Those with compromised immune systems may need to wait for twenty days to pass.
Nature: Reduced Sensitivity of SARS-CoV-2 Variant Delta to Antibody Neutralization
Emerg Inf Dis: Predictors of Nonseroconversion after SARS-CoV-2 Infection
MMWR: Reduced Risk of Reinfection with SARS-CoV-2 after COVID-19 Vaccination—Kentucky, May–June 2021
CDC: Frequently Asked Questions about COVID-19 Vaccination
11. How well does one dose of an mRNA vaccine protect me from the delta variant compared to full vaccination?
For the Pfizer, Moderna, and AstraZeneca vaccines, one dose is only 30% effective against the delta variant. That rises to 88% after the second dose of an mRNA vaccine and gradually decreases.
A comparison of antibody levels in Moderna and Pfizer recipients revealed over twice the number of antibodies produced by the Moderna vaccine. This is likely due to the increased amount of mRNA in Moderna and the longer interval between doses.
Two doses of the AstraZeneca vaccine are initially 67% effective against the delta variant. One dose of Johnson & Johnson is 64% effective against moderate to severe disease.
On November 30, 2021, there were 475 Covid cases per 100,000 unvaccinated individuals in the US. Janssen (Johnson & Johnson) recipients were 75% less likely to test positive; for Pfizer recipients, that was 80%; and for Moderna, 82%. Overall, vaccinated people were five times less likely to get Covid:

A snapshot of November 20, 2021, Covid cases reveals the relative risk of being unvaccinated. Overall, for every six people who got Covid, five were unvaccinated:
Ages 12–17: 86% unvaccinated
Ages 18–29: 73% unvaccinated
Ages 30–49: 79% unvaccinated
Ages 50–64: 79% unvaccinated
Ages 59–75: 89% unvaccinated
Ages 80+: 78% unvaccinated

If you have gotten only one dose and have been putting off finishing the series, it is very important to get that second shot. Remember, you will reach maximum immunity two weeks after the second shot.
Partially vaccinated people have a 56% greater risk of reinfection compared to fully vaccinated individuals. Only one-fifth of people who get Covid a second time are fully vaccinated.
NEJM: Effectiveness of Covid-19 Vaccines against the B.1.617.2 (Delta) Variant
Science: Durability of mRNA-1273-Vaccine-Induced Antibodies Against SARS-CoV-2 Variants
JAMA: Comparison of SARS-CoV-2 Antibody Response Following Vaccination with BNT162b2 and mRNA-1273
CDC: Rates of COVID-19 Cases and Deaths by Vaccination Status
Nature: Reduced Sensitivity of SARS-CoV-2 Variant Delta to Antibody Neutralization
12. How long does the protection from an mRNA vaccine last? Why are booster shots being recommended, and who should get one? If I got the Johnson & Johnson vaccine, should I get an mRNA booster?
Here is the rationale behind the need for an additional dose of the vaccines after six months for anyone at least 18 years old. Older teens (16 and 17) who received Pfizer are also eligible. Johnson & Johnson recipients at least eighteen years old qualify for a booster shot two months after initial vaccination:
Researchers in Israel compared people over the age of 16 who had received a booster shot to those who had only two doses of the Pfizer vaccine at least five months earlier. Among the 4,600,000 people studied, individuals without boosters were 10 times as likely to become infected with the delta variant. People at least 60 years old who received boosters at least 12 days earlier were 18 times less likely to experience severe illness and 15 times less likely to die. Waiting for the full 12 days before exposure to SARS-CoV-2 was important.
A smaller Israeli study determined that 90% of deaths among fully vaccinated people at least 50 years old occurred in those without a third dose of the Pfizer vaccine.
In a study of Covid patients without compromised immune systems, the effectiveness of the Moderna vaccine at preventing hospitalization remained steady after four months (93%). However, Pfizer recipients experienced a decline in vaccine effectiveness against illness requiring a hospital stay (91% after ten weeks to 77% after twenty weeks). The effectiveness of the Johnson & Johnson vaccine dropped from 71% to 68% after four weeks.
The efficacy of Moderna for preventing hospitalization among veterans dropped to 86% after six months. For Pfizer, that fell to 75%.
A nationwide study of all breakthrough cases among 620,000 people accessing the Veterans Health Administration during March–August 2021 showed that the Johnson & Johnson efficacy against infection dropped from 88% to 3%; for Moderna, from 92% to 64%; and for Pfizer, from 91% to 50%. The researchers attributed this decline to the increased transmissibility of the delta variant. Note that these percentages do not reflect how well a vaccine prevents hospitalization or death. This study fills a large gap in our knowledge, as the CDC stopped reporting breakthrough cases which do not result in hospitalization or death on May 1st.
MRNA vaccines protected three-fourths of fully vaccinated people in nursing homes during March 1st–May 9th. However, that dropped to just over half during June and July. Duration since vaccination and the increase in the proportion of cases due to the delta variant factor into this.
Over half of solid organ transplant recipients showed no antibody response after two shots of the Moderna vaccine. This is due to the immunosuppressive medications they must take. When those without antibodies got a third dose six weeks later, half of them developed antibodies.
A large study in Israel conducted prior to the delta variant’s arrival determined that the effectiveness of the Pfizer vaccine dropped from 90% in the general population to 71% among immunocompromised people. That is why the CDC is now recommending immediate booster shots for people in these categories:
- Been receiving active treatment for cancer
- Taking medicine to suppress the immune system after an organ transplant
- Had a stem cell transplant within the last 2 years and suppressing the immune system
- Have moderate or severe immunodeficiency due to diseases such as DiGeorge syndrome and Wiskott-Aldrich syndrome
- Has an advanced or untreated HIV infection
- Being treated with high-dose corticosteroids or other medications which may limit your immune response
More recent research in the US confirmed a decreased vaccine effectiveness to prevent hospitalization among immunocompromised people of 77% vs. 90% for those with healthy immune systems. In general, Moderna provided better protection than Pfizer. Effectiveness rates varied widely based upon the type of immune disorder. You can click here to see more specific information.
Vaccinated patients with blood cancers are at particularly high risk of severe illness or death if they become infected with SARS-CoV2 due to their inability to mount an immune response. Clinicians recommend immediate monoclonal antibody treatment should that occur.
For some immunosuppressed people, three shots of an mRNA vaccine constitute the primary series. Their fourth shot acts as the booster.
.
Typically, a vaccination series has a longer interval between doses. For example, you would receive the second dose of a vaccine to prevent shingles two to six months after the first shot. That extended period enables a greater immune response to the second dose. Since the first dose of the mRNA vaccines protected only 30% of people, waiting longer was not feasible.
.
Within the US population, the frequency and type of adverse reaction to a third shot is virtually the same as for the second dose. As with the initial series, it takes two weeks for antibody levels to reach their peak efficacy.
Another study of individuals at least 60 years old determined that a third dose of the Pfizer vaccine increased their antibody levels by an astounding 5800% in 10–19 days.
.
An analysis of Covid cases during October 2021 determined that people who had completed a vaccine series at least two weeks earlier were ten times less likely to test positive than unvaccinated individuals. Getting a booster shot doubled their protection.
A snapshot of November 20, 2021 reveals that 454 of every 100,000 unvaccinated people aged 50–64 tested positive during that week. In comparison, those who were fully vaccinated at least fourteen days earlier but had not received a booster shot were 71% less likely to test positive. Those of us who had a booster dose at least two weeks earlier were 92% less likely to get Covid.
For people over the age of 65, the difference was even more dramatic. Unvaccinated senior citizens in the US tested positive on November 20th at a rate of 636/100,000. Full vaccination dropped the risk of testing positive by 84%. Getting a booster at least two weeks before provided full protection to 96% of them.
.
Running the same analysis for death rates in November showed that people who had received booster shots were 68 times less likely to die than unvaccinated individuals.
A snapshot of deaths taken on December 4, 2021, reveals this for people aged 50–64:
- Unvaccinated = 8.26/100,000 died
- Fully Vaccinated = 0.40/100,000 died
- Boosted = 0.10/100,000 died
Full vaccination at least two weeks before even without a booster dose decreased the likelihood of death by 95%. The death rate among those with a booster shot was 99% lower than for unvaccinated people.
On December 4th, Covid death rates among senior citizens in the US were as follows:
- Unvaccinated = 44.14/100,000
- Fully Vaccinated = 3.58/100,000
- Boosted = 0.49/100,000
The death rate within that demographic for individuals at least two weeks after full vaccination was 92% lower than for unvaccinated seniors. Those with booster shots were 99% less likely to die than their unvaccinated peers.

.
You can mix vaccine types. A booster shot of the Moderna vaccine produces the strongest antibody response. People who initially received the Johnson & Johnson vaccine produced 76 times more antibodies after a Moderna booster; 35 times more antibodies with Pfizer, and 4 times more with a second Johnson & Johnson dose. It’s important to know that in that study, only the Moderna booster recipients were tested against the delta variant. Therefore, the efficacy of the Pfizer and Johnson & Johnson boosters are likely lower than they reported.
People whose primary series was the AstraZeneca vaccine followed by a booster shot of the Pfizer vaccine produced four times more antibodies than those who got a third shot of AstraZeneca. This study did not include testing against the delta variant.
CDC: COVID-19 Vaccine Booster Shots
NEJM: BNT162b2 Vaccine Booster and Mortality Due to Covid-19
CDC: Rates of COVID-19 Cases and Deaths by Vaccination Status
Clin Inf Dis: Effectiveness of the Two-Dose BNT162b2 Vaccine: Analysis of Real-World Data
CDC: COVID-19 Vaccines for Moderately to Severely Immunocompromised People
MedRxiv: Preliminary Analysis of Safety and Immunogenicity of a SARS-CoV-2 Variant Vaccine Booster
NEJM: Protection of BNT162b2 Vaccine Booster against Covid-19 in Israel
CDC: Rates of COVID-19 Cases and Deaths by Vaccination Status
MedRxiv: Heterologous SARS-CoV-2 Booster Vaccinations—Preliminary Report
.
13. How effectively do the vaccines protect us from hospitalization or death?
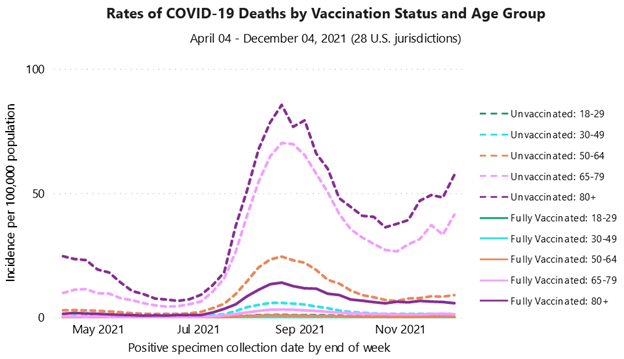
On December 4, 2021, this was the relative risk of adults dying from Covid according to vaccination status and age. Overall, for every 16 people who died, 15 were unvaccinated:
- Ages 18–29: 97% unvaccinated (0.37/0.01)
- Ages 30–49: 96% unvaccinated (1.42/0.05)
- Ages 50–64: 96% unvaccinated (9.03/0.36)
- Ages 59–75: 97% unvaccinated (41.35/1.35)
- Ages 80+: 90% unvaccinated (57.34/5.76)
As of October 18, 2021, this is what had happened in the US:
| Total number of severe vaccine breakthrough infections reported: 41,127 |
| Deaths [Total=10,857] | Hospitalized, non-fatal* [Total=30,270] | |||
|---|---|---|---|---|
| Females | 4,619 (43%) | 14,453 (48%) | ||
| People aged ≥65 years | 9,172 (85%) | 20,008 (66%) | ||
| Asymptomatic or not COVID-related | 2,299 (21%) | 7,866 (26%) |
* While most deaths were among hospitalized individuals, a small number were not.
Using almost the same procedures as in the table in Question #1, I compared all hospitalizations and deaths for unvaccinated and vaccinated people in the US during July 26th through October 18th.
The CDC defines a breakthrough infection as one occurring at least fourteen days after full vaccination.
Due to reports of missing data on vaccination status from states to the CDC regarding hospitalizations, I’ve made a worst-case assumption that the actual number may be twice the number reported and provided a range for that statistic:

- For every 14–27 hospitalizations, one person was fully vaccinated
- For every 10 deaths, one person was fully vaccinated
Over the course of the entire pandemic, 98.50% of all Covid-19 deaths occurred in unvaccinated people or prior to two weeks after full vaccination.
The CDC stopped reported detailed breakthrough information after October 18th. That is why I have not updated those statistics.
.
As the proportion of cases due to the delta variant increased from 2% to 80% in New York, the effectiveness of full vaccination to prevent infection dropped from 92% to 80%. Nevertheless, the vaccines remained equally effective at preventing hospitalization (94.5% average). For each unvaccinated person who required hospitalization, there were twelve unvaccinated patients.
Another large study found the effectiveness of the Pfizer vaccine against infection with the delta variant dropped from 88% to 47% after six months. However, protection against severe illness requiring hospitalization held steady at 93%.
In a study of Covid patients without compromised immune systems, the effectiveness of the Moderna vaccine at preventing hospitalization remained steady after four months (93%). However, Pfizer recipients experienced a decline in vaccine effectiveness against illness requiring a hospital stay (91% after ten weeks to 77% after twenty weeks). The effectiveness of the Johnson & Johnson vaccine dropped from 71% to 68% after four weeks.
The efficacy of two doses of Moderna for preventing hospitalization among veterans dropped to 86% after six months. For Pfizer, that fell to 75%.
In contrast, the effectiveness of the Johnson & Johnson vaccine against infection dropped to 3% in a nationwide study of 620,000 veterans during February 1–August 13, 2021.
During the period when the delta variant predominated, there were 90% fewer hospitalizations than expected among adults who had received a second dose of an mRNA vaccine within 14–179 days. After 180 days without a booster, Vaccine Efficacy against hospitalization dropped to 81%. Getting a booster shot dropped the need for hospital care by 94%.
Compared to unvaccinated adults in California without prior infection during October 2021:
- Vaccinated, no infection history = hospitalized 20 x less often
- Unvaccinated, prior infection = hospitalized 54 x less often
- Vaccinated, previous infection = hospitalized 58x less often
- This applies only to the delta variant
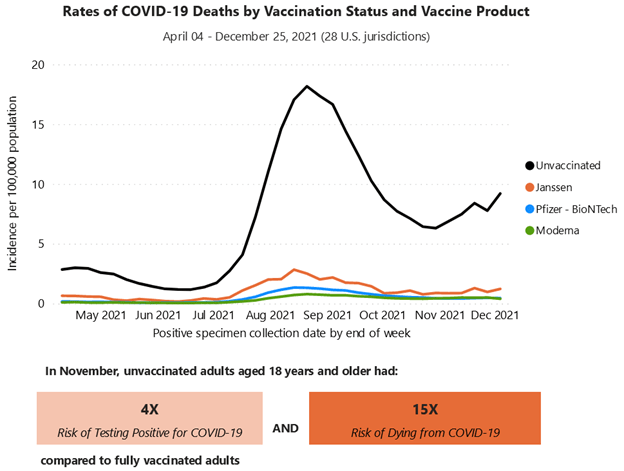
The CDC is now publishing death rates per 100,000 people by vaccine status and type. On December 4, 2021, there were 9.20 deaths per 100,000 unvaccinated individuals. Recipients of Janssen (Johnson & Johnson) were 87% less likely to die (1.22/100,0000; 95% less for Pfizer (0.46/100,000) and 96% less for Moderna (0.40/100,000). Overall, in November, unvaccinated adults were 15 times more likely to die:
In the UK, 90% of adults have received at least one dose of a vaccine. That decreases the risk of hospitalization by 96%. However, slightly more than half of deaths have occurred in fully vaccinated people.
Compare an 80-year-old fully vaccinated man with a 45-year-old unvaccinated man. The risk of death from Covid doubles with every seven years of age. Dropping the likelihood of death 20 times by being vaccinated cannot offset increasing the risk of being 80 years old by 32 times.
CDC: Rates of COVID-19 Cases and Deaths by Vaccination Status
CDC: COVID-19 Vaccine Breakthrough Case Investigation and Reporting
Politico: Holes in Reporting of Breakthrough Covid Cases Hamper CDC Response
CDC: Trends in the Number of COVID-19 Vaccinations in the US
CDC: Rates of COVID-19 Cases and Deaths by Vaccination Status
.
This series of memes adapted from an interview with a respiratory therapist gives an outstanding depiction of the difference vaccination makes:


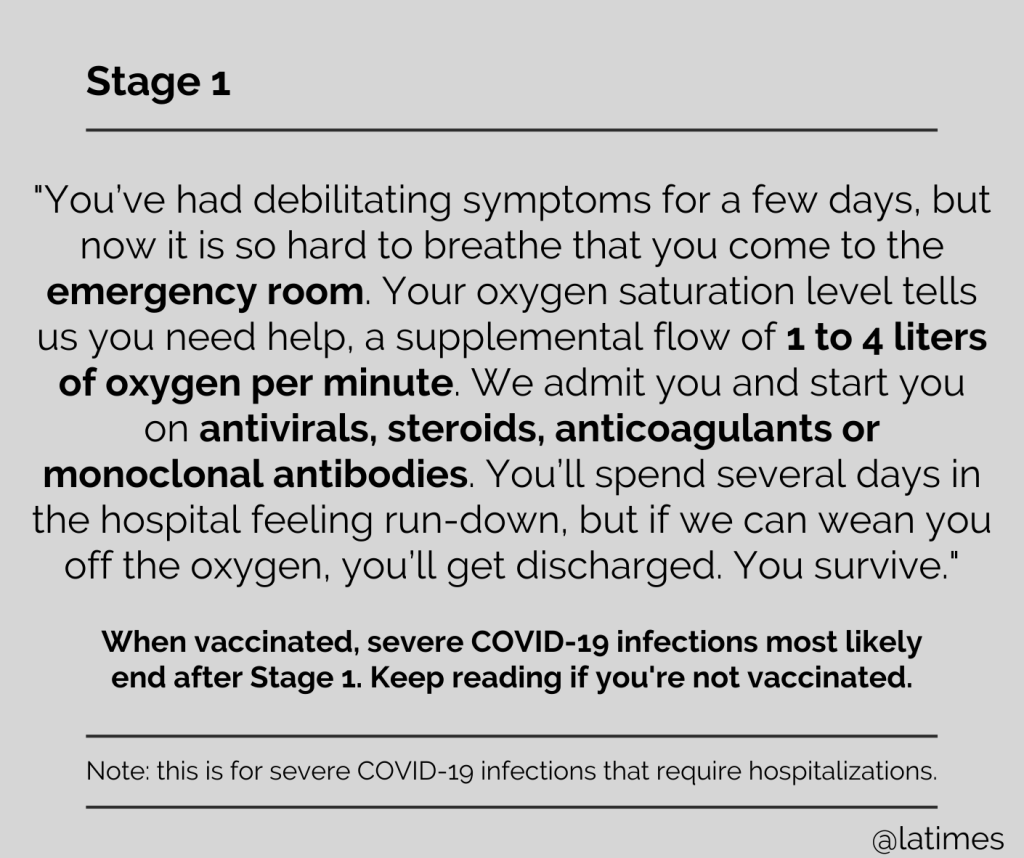
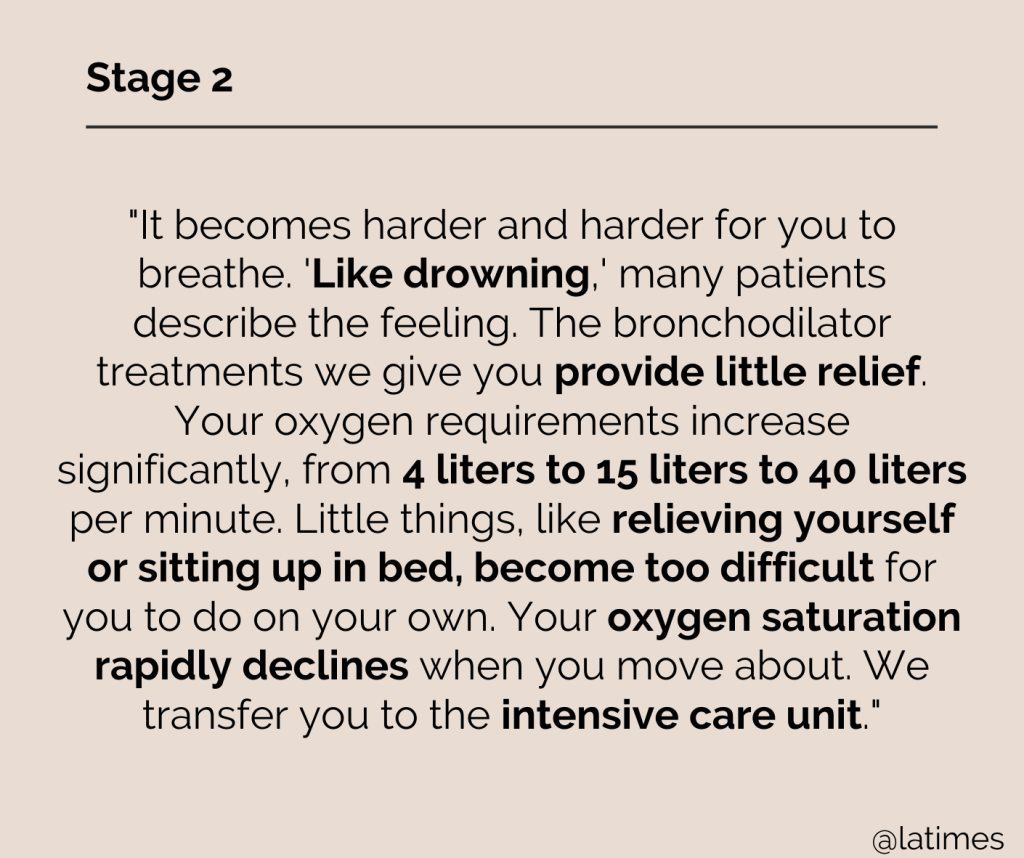






Honolulu Emergency Management: The 7 Stages of Severe Covid-19
LA Times: On the Front Lines, Here’s What the Seven Stages of Severe Covid-19 Look Like
.
14. How risky is post-vaccination myocarditis for younger people? How does the risk of other vaccine side effects compare to the symptoms of Covid?
Concerns about myocarditis and pericarditis after vaccination have prevented many young men and women from getting vaccinated. For the mRNA vaccines, they have occurred at a rate of 12.6/million.
People who experience this side effect have chest pain within 2–3 days after receiving their second dose of an mRNA vaccine. Almost all cases remained mild, and the patients fully recovered.
However, young men who become infected with SARS-CoV-2 develop those conditions at a rate of 450/million. Infected young women experience them at a rate of 235/million.
In contrast to the myocarditis arising from vaccination, the inflammation resulting from SARS-CoV-2 can cause life-threatening heart conditions in children, adolescents, and adults.

With the delta variant transmitting as easily as chickenpox, it is far safer to get vaccinated.
A nationwide study in Israel revealed that no adolescents who received two doses of the Pfizer vaccine needed hospitalization for the Covid-19 delta variant, in contrast to one in every 300 of their unvaccinated peers.
In the US during June through September 2021, the Pfizer vaccine was 93% effective at preventing hospitalization in adolescents. None of the 77 teens who required ICU admission or life support or who died were fully vaccinated.
Research into 2.4 million vaccine recipients, who were equally divided between the Moderna and Pfizer vaccine, identified fifteen men between the ages of 18 and 40 who required hospitalization for myocarditis. All responded well to standard treatment. There was no statistical difference between Moderna and Pfizer recipients (seven vs. eight).
On October 29, 2021, the FDA approved Pfizer vaccine’s Emergency Use Authorization in children 5–11 years old. It prevented 90% of SARS-CoV2 infections. Among the 3,100 children who received the vaccine, there were no cases of myocarditis, pericarditis, anaphylaxis, or death. Children who experienced fatigue, muscle pain, or headache after vaccination recovered within two days.
Circulation: Myocarditis with COVID-19 mRNA Vaccines
JAMA: Acute Myocarditis Following COVID-19 mRNA Vaccination in Adults Aged 18 Years or Older
.
A study of two million people in Israel compared the likelihood of experiencing a significant Pfizer vaccine-induced side effect to the risk of those same symptoms of Covid-19. Here are the results:

Compared to those infected with SARS-CoV-2, people vaccinated with two doses of the Pfizer vaccine were substantially protected against acute kidney injury, cardiac arrythmia, deep vein thrombosis, hemorrhagic stroke, heart attack, myocarditis, inflammation surrounding the heart, blood clots in the lung, erectile dysfunction, and reduced male fertility.
While cases of shingles remained rare among individuals in that study, there was an increase in risk among those who received the vaccine.
The Radiological Society of North America recommends waiting 4–6 weeks after the final dose of an mRNA vaccine to undergo a routine mammogram, noting that swelling of lymph nodes in the armpit (lymphadenopathy) is a normal immune response that resolves with time.
This is a side effect which I experienced. While I was aware of a lump for a few weeks, it didn’t cause any problems. Nevertheless, I did mention it to the woman who did my mammogram. She then asked which arms had received the injections in case any swelling appeared in the scans.
NEJM: Safety of the BNT162b2 mRNA Covid-19 Vaccine in a Nationwide Setting
JAMA: Sperm Parameters Before and After COVID-19 mRNA Vaccination
The Conversation: COVID-19 Could Cause Male Infertility and Sexual Dysfunction—but Vaccines Do Not
RSNA: Covid-19 Vaccine-Related Lymphadenopathy: What to Be Aware Of
.
15. Are mRNA vaccines safe for pregnant women and their babies?
Research comparing miscarriages, preterm births, and low birth weights as pregnancy outcomes for vaccinated women and women who were pregnant before the pandemic found no differences between them. No neonatal deaths occurred among vaccinated women.
Newborns whose mothers were vaccinated early in the third trimester produced a greater antibody response compared to those whose mothers received a vaccine closer to the time of delivery.
Vaccinated women who breastfed their infants secreted Covid-specific antibodies in their milk for at least six weeks. That provided protection to their newborns.
Milk from breastfeeding women who received either mRNA vaccine did not yield any detectable vaccine in the days after vaccination.
On the other hand, pregnant women who become infected with SARS-CoV-2 are more likely to experience severe illness requiring hospitalization, breathing assistance, or ventilation. They also have increased risk of preterm delivery or death.
From March 2020–October 2021, fifteen pregnant women died from Covid in in Mississippi alone. Almost all had underlying conditions and most died a few days after giving birth. None were fully vaccinated.
The delta variant increased the likelihood of death five times compared to the original SARS-CoV-2 virus, from five deaths/1,000 pregnant women with Covid-19 to 25/1,000. During the time when the delta variant predominated, pregnant women infected with SARS-CoV-2 in Mississippi were eight times more likely to die than infected women of similar ages who were not expecting a child. Black and Hispanic women were at greatest risk.
A study of 1,250,000 births in the US from March 2020 through September 2021 found that pregnant women infected with the delta variant are four times as likely to experience stillbirth as uninfected women. Investigators in this study were not able to assess their vaccination status. As of July 2021, only 30% of pregnant women were fully vaccinated.
That is why the American College of Obstetrics and Gynecology enthusiastically recommends that all pregnant women receive vaccination and Pfizer booster shots, and the CDC has issued an urgent advisory.
Similar results occur with the AstraZeneca vaccine, and a second dose is recommended for women who become pregnant after starting the series. However, due to more research on pregnancy with the mRNA vaccines, Pfizer or Moderna are preferable for unvaccinated women.
NEJM: Preliminary Finding of mRNA Covid-19 Vaccine Safety in Pregnant Persons
NEJM: Receipt of mRNA Vaccines and Risk of Spontaneous Abortion
JAMA: Spontaneous Abortion Following COVID-19 Vaccination During Pregnancy
JAMA: Evaluation of Messenger RNA from COVID-19 BTN162b2 and mRNA-1273 Vaccines in Human Milk
CDC: COVID-19 Vaccines While Pregnant or Breastfeeding
ACOG: COVID-19 Vaccination Considerations for Obstetric–Gynecologic Care
Royal College of Obstetricians and Gynaecologists: Covid-19 Vaccines, Pregnancy, and Breastfeeding
.
16. What about the risk of infertility?
Women may experience irregular menstrual cycles or changes in flow after vaccination or after having Covid-19. This is common for infections and immune system reactions and lasts for only a few months. The North American Society for Pediatric and Adolescent Gynecology recommends vaccination for adolescents and young adults.
A recent study confirmed that antibodies to the SARS-CoV-2 spike protein have no effect upon the implantation of an embryo or pregnancy development. In women, neither natural infection nor vaccination cause sterility.
Another study involving sperm counts in men found that sperm concentration and motility increased after the second vaccination. In contrast, research on men who contracted Covid-19 found reduced fertility and erectile dysfunction.
ASRM: New Study Reveals Covid Vaccine Does Not Cause Female Sterility
Royal College of Obstetricians and Gynaecologists: Covid-19 Vaccines, Pregnancy, and Breastfeeding
JAMA: Sperm Parameters Before and After COVID-19 mRNA Vaccination
The Conversation: COVID-19 Could Cause Male Infertility and Sexual Dysfunction—but Vaccines Do Not
.
17. How can I discuss this with people I love who are vaccine-hesitant?
Here is an explanation I gave to a friend who had been terrified about getting vaccinated until a mutual friend got Covid:
The day of our friend’s diagnosis, she got vaccinated but called me the next day because she wasn’t feeling great. I explained the vaccine to my friend using coral snakes and milk snakes to illustrate:
“Your immune system is encountering what it thinks is a coral snake and is rising up to kill it. If you’re not feeling good, it’s because your immune system is working to destroy a coral snake. Since there’s no genetic material there, it can’t reproduce, and it does not affect your DNA. Within a few days your liver clears out what’s left.
“Right now, you’re 30% protected from the delta variant. When another milk snake comes along, your immune system produces more protection to destroy what looks like the same threat.
“Two weeks after the second dose, when your immune system sees a coral snake, it’s prepared to overwhelm it before it can make you very sick. Based on what I’m seeing, most of the antibodies are in lymph nodes in your chest. That explains why fully vaccinated people who do get infected usually have mild cold symptoms. The virus gets neutralized before reaching your lungs.”


MedLine Plus: What are mRNA Vaccines and How Do They Work?
Ad Drug Deliv Rev: Controlling Timing and Location in Vaccines
UAB: Three Things to Know about the Long-Term Side Effects of COVID Vaccines
.
18. What sources can I trust?
1) Health Data.Gov – COVID-19 Community Profile Report – Updated every weekday
2) World Health Organization Situation Reports – These tend to be one day behind. Some nations are not keeping their information up to date:
3) Johns Hopkins University – Johns Hopkins Univ: Coronavirus Resource Center. Not recommended for Florida statistics as that state updates only once per week, is hiding deaths, and does not include any non-resident data.
4) MedPage Today – MedPage Today: Covid -19 Updates
5) Investigation of SARS-CoV-2 Variants of Concern: Technical Briefings – for the UK
6) Redemptive History and Theology – Covid-19 Information covers broader Covid-19 issues, including medical and theological perspectives
7) HHS Protect Public Data Hub – Hospital Utilization by facility or by state
8) CDC: Covid-19 Integrated County View – transmission, cases, test positivity, deaths, hospital usage, % of vaccinated people, and a Social Vulnerability Index by county
9) Florida Statistics: What is Really Happening? – A review of Florida statistics showing what that state is trying to hide and how you can find the missing information.
10) Dr. Jason Salemi – Covid-19 Dashboard: A Focus on FL with National Comparisons
Image via Wikimedia Commons

