This post is archived. You can access my most recent post here.
About me: I have a masters’ degree in Infectious Disease Epidemiology from UCLA, a bachelors’ degree from Wheaton College in biology with a certificate in International Community Development, and a masters’ in Greek and Hebrew Exegesis from Gordon-Conwell Theological Seminary. Usually, I am writing and posting bible studies on the Redemptive History Facebook page, but these are not normal times.
I began my career by editing a medical monograph and writing an accompanying peer-reviewed journal article during my graduate studies at UCLA (MPH, Tropical and Infectious Disease Epidemiology). My first publication concerned the excess risk of severe illness or death from a bacterium in raw milk in California. It was featured on the front page of the Los Angeles Times and was debated in the state legislature.
After graduation, I conducted records-based research concerning the efficacy of a poly-pharmacy reduction program for nursing home residents. We focused upon the frequency and severity of adverse drug reactions, and whether our patients could stop taking their medications without needing to resume using them. Textbooks still cite it today.
Paul Terrill MD, FAAFP has been an invaluable collaborator in assessing and compiling many of these resources.
Due to the sudden onset and severity of the pandemic, many journals are pre-empting their normal four-week to six-month process of peer reviewing articles before releasing them for publication. When you look at any research involving Covid-19, it is important to note the status of the article: pre-print or accepted for publication after peer review. Check the comments under pre-print articles. Several major studies were retracted after the peer-review process detected significant issues.
Lancet, NEJM retract studies on hydroxychloroquine for COVID-19
For information specifically about the delta variant, click here.
This post addresses these issues:
What are the symptoms for Covid-19? How is “long haul” Covid-19 different from most cases?
What do we know about how Covid-19 is transmitted from person to person?
Who can transmit the virus?
Who gets sickest?
How do medications and supplements affect this disease?
Face Coverings and Covid-19
What does “flattening the curve” mean? How do we do that?
What is the difference between social distancing, self-quarantine, and isolation?
How long will this last? What about vaccines?
What should we do and what should we avoid?
A reflection by Kelly Ladd Bishop
A letter from Martin Luther
____________________________________________________________________________________________
What are the symptoms for Covid-19? How is “long haul” Covid-19 different from most cases?
People with COVID-19 have had a wide range of symptoms reported – from no symptoms to severe illness.
Fever, cough, congestion, runny nose, fatigue, chills, muscle pain, sore throat, shortness of breath, headache, chest pain, or a new loss of taste or smell can occur 2–14 days after exposure. People who lose their sense of smell typically experience a milder form of the disease. Some patients experience nausea, vomiting, or diarrhea.
People infected with the delta variant are less likely to experience cough or the loss of smell. The loss of smell usually accompanies a milder infection, so this does fit with the increased virulence we are now seeing. Delta variant infections often produce a headache, runny nose, sore throat, congestion, sneezing, muscle pain, and fever.
As of August 21, 2021, 99% of SARS-CoV-2 infections in the US are due to the delta variant.
Mayo Clinic Coronavirus disease 2019 (COVID-19)
Smell loss is a prognostic factor for lower severity of coronavirus disease 2019
Symptoms which require immediate emergency medical care include difficulty breathing, continuous pressure or pain in the chest, an inability to awaken or to stay awake, a new onset of confusion, or a blue tinge in the face or lips.
Investing in a pulse oximeter to track your blood oxygen level is a great idea. They cost about $20. A normal oxygen saturation level runs between 95–100%. People with Covid-19 can experience a drop in that percentage without realizing it has happened. If it does occur, seek medical attention immediately.
In serious cases, people have the fever and cough for about a week before breathing problems develop. The virus works by shutting the immune system down and stripping away the lung lining. In some people, the immune system then kicks in with what is called a “cytokine storm” of interleukin-6. It can be as deadly as the virus, damaging the lungs, heart, liver, kidneys, and brain.
The First Shot: Inside the Covid Vaccine Fast Track
The Lancet: COVID-19: consider cytokine storm syndromes and immunosuppression
Recently, researchers have begun investigating another aspect of a person’s system which can go awry when it encounters SARS CoV-2. Covid-19 patients can have up to 200 times the normal number of angiotensin-converting enzyme 2 (ACE2) receptors which the virus uses to enter a cell. When the virus encounters an ACE2 receptor, increases in interleukin-1 and interleukin-6 cause an abnormal response in the bradykinin system.
Covid-19 patients also have less angiotensin-converting enzyme (ACE) to break down bradykinins, large amounts of hyaluronic acid—a polymer which can hold 1000 times its weight in water—and fewer genes to remove hyaluronic acid. When the bradykinin system gets out of control, blood vessels expand and begin to leak.
This theory connects many of the odd symptoms which occur in Covid-19: abnormal blood clotting; a fluid the consistency of gelatin forming in the lungs; and difficulty transporting oxygen from the lungs to the bloodstream and other organs. Too much bradykinin also causes a shift in a person’s electrolytes, such as potassium. That leads to excess fluid throughout the body, sudden death due to cardiac arrest, diarrhea, and confusion. Too little ACE causes the loss of taste and smell.
Patients with gastrointestinal symptoms, such as abdominal pain or GI bleeding can have Covid-19 as the underlying cause. These tend to be more severe cases.
Recently, concern has arisen about a post-viral condition in Covid-19 patients called myalgic encephalomyelitis. It results in exhaustion, difficulty thinking, muscle pain, and headaches.
STAT: Chronic fatigue syndrome may hold keys to understanding post-Covid syndrome
CDC: Myalgic Encephalomyelitis/Chronic Fatigue Syndrome
Two months they were diagnosed with Covid-19, three-fourths of patients undergoing heart evaluations showed cardiac injury. Over half still had cardiac inflammation. One-fifth continued to have excess fluid around the heart or scar tissue in it. The swelling and scarring could cause cardiac issues even ten years from now.
After examining multiple studies, a group of cardiologists recommends cardiac testing for athletes with moderate to severe Covid-19, people with symptoms which last more than nine days, athletes who resume training and experience Covid-19 symptoms, and all athletes aged 65 and over.
In general, people who have tested positive for SARS CoV-2 can resume exercising ten days after their symptoms disappear.
Research from the Diamond Princess cruise ship revealed that almost half of infected passengers remained asymptomatic. What is particularly worrisome is that most of the CT scans performed on asymptomatic individuals revealed the characteristic “ground glass opacity” characteristic of Covid-19. How this will affect them in the years to come remains unknown.
Ann Intern Med: Prevalence of Asymptomatic SARS-CoV-2 Infection
Other people might appear to be asymptomatic because they exhibit no respiratory symptoms associated with SARS CoV-2 infection. However, they develop a wide range of neurological problems, such as delirium, psychosis, peripheral neuropathy, encephalitis, confusion, or stroke. Approximately one-third of Covid-19 patients develop lingering neurological effects which affect their ability to think clearly.
Even relatively young people with mild or no symptoms are experiencing major strokes typical in elderly people. A Dutch study found that one-third of Covid-19 patients in the ICU experienced blood clotting disorders, including strokes, deep vein thromboses, pulmonary embolisms, and heart attacks.
Brain: The emerging spectrum of COVID-19 neurology: clinical, radiological and laboratory findings
NEJM: Large-Vessel Stroke as a Presenting Feature of Covid-19 in the Young
Researchers are investigating the effects of Covid-19 on male fertility, as the Angiotensin Converting Enzyme 2 receptor sites for the virus are also located in testicles. The concentration of this enzyme peaks at the age of thirty. Most of the damage found in autopsies resulted from inflammation. In one study, one-fifth of male patients reported scrotal or testicular pain.
World J Urol: Does COVID-19 affect male fertility?
Am Soc Reprod Med: SMRU Statement Regarding Male Reproductive Health and COVID-19
Various skin rashes occur in Covid-19 patients.
Some children and young adults who test positive are developing red lesions on their feet and toes. This may be their only symptom. They almost never test positive for active infection and only one-fourth develop antibodies. However, with similar patients, biopsies of these toe lesions showed the crown characteristic of the SARS CoV–2 virus’s spike, providing us with a definitive diagnosis of Covid-19 infection.
Amer Acad Dermatol: COVID toes, rashes: How the coronavirus can affect your skin
Cleveland Clinic: Skin Rashes: An Emerging Symptom of COVID-19
Univ Wisconsin studying ‘COVID toes,’ skin condition apparently linked to COVID-19
Int J Dermatol: Chilblain‐like lesions on feet and hands during the COVID‐19 Pandemic
A small percentage of children with Covid-19 require hospitalization for an extreme inflammatory response akin to toxic shock. It affects the heart, kidney, gastrointestinal tract, blood, skin, mucous membranes, and nervous system. They may have remained asymptomatic while the virus was actively replicating inside them and then developed Multisystem Inflammatory Syndrome 3–4 weeks they were infected. Many of such children had negative tests for active virus but positive tests for antibodies to SARS CoV-2.
As of October 4, 2021, 5,217 such patients have been reported in the US. This Multisystem Inflammatory Syndrome disproportionally affects Hispanic and Black children. Two-thirds of children who develop MIS-C had no underlying medical conditions prior to infection with SARS-CoV-2. At least four organ systems were affected in 86% of these children, with some having difficulty in six types. Two-thirds required care in the ICU and forty-six children died.
Lancet: Multisystem inflammatory syndrome in children: A systematic review
My friend’s teen daughter required oral surgery after inflammation caused her gums to grow over her molars. Physicians are now reporting these symptoms in young adults, with increasing severity with increasing age.
The Hill: Doctors say they are seeing coronavirus-linked inflammatory disease in some young adults
Am J Emerg Med: COVID-19 associated Kawasaki-like multisystem inflammatory disease in an adult
If you or a family member are sick and think it might be Covid-19, call your doctor. Do not just go to the clinic, as you will infect others.
Mayo: Coronavirus disease 2019 (COVID-19)
Emory University has developed an online tool to check whether what you are experiencing matches the symptoms for Covid-19. It’s available here.
This is not “just the flu.” Between February 1, 2020, and August 21, 2021, the number of deaths due to Covid-19 were sixty-six times those due to influenza (623,997 vs. 9,415). Note that this information can take more than eight weeks to be included in the national database.
How is “long haul” Covid-19 different from most cases?
Some patients are experiencing different symptoms of Covid-19 in sequence over many weeks, often a few days after they begin feeling better. One person I know was quite ill for three-months before starting to feel better. She began with cardiac issues, then gastrointestinal, then painful breathing, then post-viral syndrome, a deep vein thrombosis, and most recently returned to more severe gastrointestinal problems. In all, she made thirteen trips to the emergency room.
A survey of people who fall into this category reveals some startling information. Most of the respondents were white women, which could result from being willing and able to take a survey. Note that most patients had not yet reached the 7th week of illness.
Confirming that everyone needs to take this coronavirus seriously, almost two-thirds of “long haul” patients were between the ages of 30 and 49. Ninety percent of the respondents remained ill when they completed the survey.
These patients experience an enormous decline in their physical activity levels, with 67% describing themselves as at least moderately physically active prior to becoming ill. Since becoming infected, 65% call themselves—at best—mostly sedentary. In the case of my friend, she used to hike in the mountains for five hours at a time. For months after becoming infected, a thirty-minute walk kept her in bed the next day.
Almost half of long-haul patients were never tested because they did not meet the testing criteria or test kits were not available. Among those who did receive testing, 54% tested negative. Most of the 46% who tested positive were tested early in the course of their illness. Both groups had similar symptoms, with only the loss of taste and/or smell occurring more frequently in the positive patients.
While over half of the survey respondents reported at least one preexisting condition, only asthma showed a correlation with a lengthy recovery time. Among the patients who knew their blood type, O+ and A+ appear a bit protective for this form of the disease when compared to the distribution of blood types in the US and UK. The B and Negative blood groups were slightly over-represented, with B- the most extreme.
Most of these patients did not require a hospital admission. However, many sought Emergency Room care, some repeatedly.
Typically, they began with gastrointestinal symptoms and chills/sweating during the first two weeks. Respiratory symptoms started during the third and fourth weeks. In all, they reported over 200 different symptoms. The most common included a dry cough, loss of appetite, a tight chest, difficulty breathing, fever of at least 100.1 degrees, gastrointestinal problems, burning in the lungs, an increased heart rate, brain fog, an inability to concentrate, and dizziness.
Eighty-nine percent of these patients reported changes in the intensity and frequency of their symptoms, while 70% noted that new symptoms arose at different times. One patient wrote that it was like playing “Whack-a-Mole.” As soon as one symptom subsided, a new one arose.
A professor at the Liverpool School of Tropical Medicine described his seven weeks of illness:
In the first days at home I wasn’t sure I had Covid-19. Then I damaged my hands with bleach…I could not smell the chlorine. The heaviness and malaise became worse, I had a tightness in the chest, and realised it could be nothing else…One afternoon I suddenly developed a tachycardia, tightness in the chest, and felt so unwell I thought I was dying. My mind became foggy. I tried to google fulminating myocarditis but couldn’t navigate the screen properly…A few hours later I woke up, alive, and the tightness replaced by extreme fatigue…
The illness went on and on. The symptoms changed, it was like an advent calendar, every day there was a surprise, something new. A muggy head; acutely painful calf; upset stomach; tinnitus; pins and needles; aching all over; breathlessness; dizziness; arthritis in my hands; weird sensation in the skin with synthetic materials. Gentle exercise or walking made me worse. I would feel absolutely dreadful the next day….
A large study in the US revealed that over one-third of people who tested positive for SARS-CoV-2 continued to experience at least one symptom three to six months after being diagnosed.
The most common long-lasting symptoms include fatigue, muscle or joint pain, difficulty breathing, chest pain, brain fog, coughing, the inability to taste, and the loss of smell.
PLoS Med: Incidence, Co-occurrence, and Evolution of Long-COVID Features: A 6-Month Retrospective Cohort Study of 237,618 Survivors of COVID-19
JAMA: As Their Numbers Grow, COVID-19 “Long Haulers” Stump Experts
What do we know about how Covid-19 is transmitted from person to person?
The RNA in the SARS CoV-2 virus mutates every two or three times it replicates. These changes are simple errors in the genetic code. Researchers can sequence the RNA from 100 infected individuals in a few days. This enables genomic epidemiologists to determine whether the infections in a cluster of cases are related and, if so, who infected whom.
Bloomberg: Who Infected the President?
Transmission occurs through respiratory droplets, surface contact, and possibly via blood or by flushing the toilet.
The CDC has upgraded their warning to state that the virus spreads very easily between people, with transmission increasing in correlation with how close they are and how long they remain together. They note that it may also spread by contacting a contaminated surface and then touching your eyes, nose, or mouth.
In a study in Singapore, about half of the people who tested positive for Covid-19 exhibited no symptoms. Although those without symptoms have fewer opportunities to spread the virus by coughing or sneezing, some people in this category have spread the infection to others. This was especially true within households.
Reuters Exclusive: Half of Singapore’s new COVID-19 cases are symptomless – taskforce head
Active virus also occurs in blood plasma, even among asymptomatic people who test positive.
Emerg Infect Dis: Severe Acute Respiratory Syndrome Coronavirus 2 RNA Detected in Blood Donations
Researchers have recovered the virus from 41% of stool samples taken from patients with gastrointestinal symptoms.
A study of patients who underwent semen testing found the virus in 27% of men at the height of their symptoms. That dropped to 9% as they began recovering. Other researchers found no active virus in the semen after an average of a month from symptom onset. While we currently have no evidence of sexual transmission, that possibility does remain given the presence of SARS Cov-2 in semen samples.
Am Soc Reprod Med: SMRU Statement Regarding Male Reproductive Health and COVID-19
Aerosols are small enough to reach deeply into our lungs. We produce aerosols when singing, speaking loudly, or yelling. A recent experiment indicates that one minute of loud speech by a person infected with the coronavirus can produce 1,000–100,000 aerosols containing the virus which can remain airborne for up to eight minutes. Sneezing can yield 40,000 aerosols, while coughing can create 3,000. The viral particles in an aerosol remain infectious for up to sixteen hours.
Testing under various temperatures and humidities revealed that the aerosols generated by a sneeze or cough can travel up to twenty-seven feet. This enables the coronavirus to infect people farther than six feet away and to travel through ventilation systems.
MIT News: In the cloud: How coughs and sneezes float farther than you think
Singing creates six times the number of aerosols produced by normal speech. This creates a significant safety hazard for churches. After two choir practices with an infected person, 87% of the attendees developed Covid-19.
Sci Reports: Aerosol emission and superemission during human speech increase with voice loudness
“Singing, the Church, and COVID–19: A Caution for Moving Forward in Our Current Pandemic” provides an outstanding examination of the issues surrounding congregational and choral singing.
Singing, the Church, and COVID-19: A Caution for Moving Forward in Our Current Pandemic
Viral transmission also depends upon how long an uninfected person is exposed to someone carrying the virus. Based upon research into similar viruses, the amount of virus necessary to produce an infection could be as little as 100 particles. The respiratory fluids of sick people contain between 1,000,000 and 100,000,000 particles per milliliter. Decreasing the number of people in a room also lowers the likelihood of contact with an infected individual.
Sci Media Ctr: expert reaction to questions about COVID-19 and viral load
We are seeing more Covid-19 infections than expected in our homes, churches, workplaces, restaurants, parties, and on public transportation. Indoor spaces with poor ventilation account for most outbreaks. This chart comes from an outstanding article which reviews many different facets of aerosol and droplet transmission of SARS-Cov-2:

BMJ: Two metres or one: what is the evidence for physical distancing in covid-19?
Another site ranks thirty-six activities on a scale of 1–10. Note that “Dentist’s Offices 4/10” likely refers to sitting in the waiting room. The CDC has published guidelines specific to dental care.
Doctors rank these activities as most likely to spread coronavirus
CDC: Guidance for Dental Settings
Resuming Care-Filled Worship and Sacramental Life During a Pandemic provides outstanding guidelines for re-opening churches with a focus upon safety:
Resuming Care-Filled Worship and Sacramental Life During a Pandemic
This virus can survive at levels high enough to cause infection for 4 days on polystyrene, 3 days on other plastics, 3.5 days on glass, 2 days on stainless steel, and 1 day on cardboard.
Ultraviolet light rapidly degrades SARS CoV-2. If these materials remain in the dark at 68 degrees F (20 C), the virus survives for 28 days. When the researchers increased the temperature to 86 degrees F (30 C), the viability of the virus in the dark dropped to 21 days on paper money; to 7 days on glass and steel; and to 3 days on vinyl and cotton.
MMWR: Prolonged Infectivity of SARS-CoV-2 in Fomites
NEJM: Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1
Virology Journal: The effect of temperature on persistence of SARS-CoV-2 on common surfaces
SARS Cov-2 remains viable as an aerosol for sixteen hours. This makes airborne particles a major mode of transmission. In warmer, humid weather, these times decrease, which is why researchers expect another wave of transmission to begin the fall.
Emerg Inf Dis: Persistence of Severe Acute Respiratory Syndrome Coronavirus 2 in Aerosol Suspensions
A recent study indicates that the SARS CoV-2 virus remains active on human skin for nine hours. Frequent hand washing, not touching your face, and showering after potential exposure remain critically important. While a solution of 80% alcohol inactivated the virus in fifteen seconds, most hand sanitizers in the US are 60% alcohol and isopropanols (rubbing alcohols) are 70% solutions, so that finding may not apply here.
What to wipe down daily in your own home: remote controls, alarm clocks, phones, cabinet and drawer handles, doorknobs and door locks, light switches, desk surfaces, keys, credit cards, garage door opener, and refrigerator handles. Keep wipes in your car and use them every time you return. Be aware that a pet can carry the virus on its fur or skin. A few cases of infected pets have been reported, but this is rare.
WaPo: This is everywhere you should be sanitizing in your hotel
Mayo: Can COVID-19 (coronavirus) spread through food, water, surfaces and pets?
Here is a helpful post concerning how to do laundry when someone in your household is sick or may have been exposed to the virus:
Cons Rep: How to Prevent the Spread of COVID-19 While Doing Laundry
Who can transmit the virus?
People without symptoms can transmit the virus before getting sick or without getting sick at all. In a recent study of a nursing home, 67% of pre-symptomatic and asymptomatic patients tested positive for the coronavirus with large amounts of viral RNA. This fits with other research which estimates that 44% of new infections result from contact with a person who does not yet show symptoms of Covid-19.
NEJM: Presymptomatic SARS-CoV-2 Infections and Transmission in a Skilled Nursing Facility
Nat Med: Temporal dynamics in viral shedding and transmissibility of COVID-19
Viral shedding continues for approximately ten days after symptom onset in mild or moderate cases. People with severe cases or with compromised immune systems can remain contagious for up to twenty days.
CDC: Duration of Isolation and Precautions for Adults with COVID-19
Higher percentages of cases have been shifting toward younger people as time progresses, likely due to a lack of social distancing.
CDC: Demographic Trends of COVID-19 cases and deaths in the US reported to CDC
Children under ten years old are less likely to develop Covid-19. Most likely, this is because they have fewer receptors for the SARS Cov-2 virus in their nasal cavities than older children and adults do.
However, if they do become infected, even asymptomatic children shed as much of the virus detected in hospitalized adults with severe symptoms.
JAMA: Nasal Gene Expression of Angiotensin-Converting Enzyme 2 in Children and Adults
J Ped: Pediatric SARS-CoV-2: Clinical Presentation, Infectivity, and Immune Responses
The American Academy of Pediatrics reports an increasing percentage of children who test positive. Overall, 10% of reported cases occurred in children. However, that percentage increased rapidly in the eight weeks before September 10th. During the week ending on April 23rd, 3% of cases were pediatric. Beginning on July 16th, children represented 12–15.9% of new cases each week.
CDC data indicates this increase did not occur due to more testing in children relative to the rest of the US population. The percentage of tests administered to people at ages 0–17 has remained at 5–7% of all people tested since late April.
The experiences of people attending a summer camp inadvertently provided a real-world test of how well children can infect other people. Camp policy required only staff to wear masks. After two weeks, 44% of campers and staff tested positive for SARS Cov-2, with decreasing infection rates with increasing age (51% positive for children aged 6–10 years; 44%, for children aged 11–17 years; and 33%, for adults aged 18–21).
A new dashboard tracks confirmed cases in elementary schools through colleges. While the information remains incomplete, I was able to find the number of cases in our district schools.
Keeping everyone home is critically important, even when they do not feel sick. Asymptomatic carriers can infect others for longer than fourteen days. In keeping with many epidemiologists, the CDC director estimates that only 10% of infections in the United States have been identified.
Ann Int Med: Prevalence of Asymptomatic SARS-CoV-2 Infection
The Hill: CDC: Coronavirus may have infected 10 times more Americans than known
Given how difficult it is to meet the requirements to get tested, this suggests that many people who have the disease are getting false negative results. This is also likely why some people test positive, then negative, and then positive again. The second test would have been a false negative.
NEJM: False Negative Tests for SARS-CoV-2 Infection — Challenges and Implications
A study of how long antibodies to SARS Cov-2 last in people with mild cases revealed a half-life of 36 days. Another research team revealed the presence of antibodies which neutralized the virus’s protein spike for five months in over 90% of people who tested positive for the virus.
NEJM: Rapid Decay of Anti–SARS-CoV-2 Antibodies in Persons with Mild Covid-19
AAAS: Robust neutralizing antibodies to SARS-CoV-2 infection persist for months
What we do not know is how well a Covid-19 patient’s B and T cells will produce new antibodies when they encounter the virus in the future. Theoretically, they should provide protection to the same strain of SARS Cov-2 and at least partial protection to other strains.
However, there have been only a few cases of people developing Covid-19 twice, each time with a different strain of the virus. One patient had fewer symptoms the second time, which is what we would expect. Yet, another had a more severe second case. Most likely, his immune system reacted in coordination with the virus, rather than against it. Just like with influenza, an annual shot may be necessary to prevent getting infected with this coronavirus and then passing it to other people.
AP: Virus antibodies fade fast but not necessarily protection
Nature: Coronavirus reinfections: three questions scientists are asking
For each state in the US, you can track the number of new cases, the number of tests per 1,000 people, and the percentage of positive tests for the last two weeks:
JHU: Track Trends in COVID-19 Cases and Tests
CDC: United States COVID-19 Cases and Deaths by State
Raising a new concern, researchers have successfully infected deer mice in the lab by having them inhale SARS Cov-2. This is the first potential wild animal reservoir known in the US.
Who gets sickest?
Provisional death counts for February 1, 2020 through September 4, 2020 give us the number of people who have died with Covid-19 stratified by their ages and gender. Note that it takes up to eight weeks for a death certificate to be issued.
As of September 4th, 2020, the CDC reported that ages were available for 138,651 people who died from Covid-19 in the United States: <0.1% of patients aged 0–4 died (31); <0.1% of patients aged 5–17 died (50); <0.1% of patients aged 18–29 (710); 0.2% of patients aged 30–39 died (1,866); 0.6% of patients ages 40–49 died (4,744); 2.3% of patients aged 50–64 died (21,735); 8.5% of patients aged 65–74 died (29,334); 18.3% of patients aged 75–84 died (36,542); and 29% of patients at least 85 years old died (43,893).
CDC: Demographic Trends of COVID-19 cases and deaths in the US reported to CDC
JHU: Covid-19 Global Dashboard
In Florida as of September 4th, nursing home patients and staff accounted for 40% of Covid-19 deaths (4,807 of 11,963).
FL Community Dashboard: Care Facilities
FL Community Dashboard Home Page
Within the US, not enough patients had their ethnicity recorded for me to feel comfortable including those statistics here, although the CDC does report them. The US Department of Health and Human Services began requiring this information on August 1st.
As of September 4th, that information was available for only 50% of cases and 82% of deaths. Native American, Black, and Hispanic patients are disproportionally affected by Covid-19. This likely results from underlying health conditions, types of work, access to health care, how much space each person has in a home, and whether they live with multiple generations.
CDC: Demographic Trends of COVID-19 cases and deaths in the US reported to CDC
Mayo: Why are people of color more at risk of coronavirus complications?
Gender data was available for 4,518,913 Covid-19 patients (97%) in the US. Of those 51.8% of cases occurred in women. However, 54% of the people who died were men.
CDC: Demographic Trends of COVID-19 cases and deaths in the US reported to CDC
A 2019 study of women (XX), men (XY), and men with Klinefelter’s Syndrome (XXY) indicates that having two X chromosomes protects against a cytokine storm, the immune system condition associated with an increased death rate in Covid-19 patients.
Between March 1st and August 29th, nearly 0.1% of the US population had been hospitalized with Covid-19. The hospitalization rate increases as people age. For every 100,000 people aged 0–4, 16 were hospitalized; for ages 5–17, 9; for ages 18–29, 69; for ages 30–39, 108; for ages 40–49, 162; for ages 50–64, 241; for ages 65–74, 328; for ages 75–84, 516; and for those over 85, 793. That means nearly 0.8% of all Americans over the age of 85 have required hospitalization for Covid-19.
CDC: COVIDView a Weekly Surveillance Summary of US COVID-19 Activity
In one study, 39% of Covid-19 patients admitted to hospitals required mechanical ventilation for a median of nine days. Approximately half of ventilated patients will develop a condition called Post-Intensive Care Syndrome (PICS). People with diabetes, hypertension, asthma, and chronic obstructive pulmonary disease are more likely to experience the declines in their physical strength, cognition, and mental health associated with PICS. Up to 80% of them will require admission to a rehabilitation center or skilled nursing facility within two years.
During March 28th through August 29th, the CDC reported 190,912–253,841 more deaths from all causes than expected in the US, an increase of 11% despite the lag in reporting of individual deaths by up to eight weeks.
CDC: Excess Deaths Associated with COVID-19
The CDC is also reporting the location where a person died from Covid-19 for the entire US and by state. That table is much easier to interpret; however, it does not indicate whether a person who contracted the disease in a nursing home died at the hospital.
CDC: Provisional COVID-19 Death Counts by Place of Death and State
A CDC map enables you to hover over a state to see the number of reported cases and deaths there. Clicking on it will take you to that state’s health department web site for additional information.
CDC: United States COVID-19 Tracker Cases and Deaths by State
For those of you looking for Covid-19 information in Florida, I highly recommend using information from the CDC and DHHS, as the state has shut down Florida’s dashboards. Instead, the Dept of Health is releasing a report only on Fridays while omitting information on non-residents and hospitalizations. Where deaths occur within the state is withheld unless a county reports more than ten Covid fatalities during that week.
HealthData.Gov: COVID-19 Community Profile Report
Florida Health: Weekly Florida Covid-19 Data
An early study in China found that 13% of cardiac patients died, compared to 9% of diabetics; about 8% of those with COPD or hypertension died.
Worldometer: Age, Sex, Existing Conditions of COVID-19 Cases and Deaths
Obesity (BMI>29) has emerged as a major risk factor for severe illness and death. One study found that obese individuals were over seven times as likely to require critical care.
Diabetes Metab Synd: Obesity as a predictor for a poor prognosis of COVID-19: A systematic review
Chronic kidney disease, liver disease, sickle cell disease, and immunocompromisation—from an organ transplant or from being over 65 years old—also carry increased risk.
CDC: People at Increased Risk And Other People Who Need to Take Extra Precautions
CDC: Older Adults At greater risk of requiring hospitalization or dying if diagnosed with COVID-19
One small study of active and recent cancer patients examined the Covid-19 death rates for those admitted to the ICU. People with hematologic cancers, such as lymphoma and leukemia, were almost twice as likely to die than patients with solid tumors, such as breast or lung cancer (47% and 27% respectively).
Other research has found that 29% of all Covid-19 patients admitted to an ICU died, so having a solid cancer likely presents little increased risk of death.
MedPage: COVID-19 Plus Cancer Proves Deadly — Over a third of cancer patients sent to the ICU died
A review of fifty-two studies involving death rates among cancer patients with Covid-19 found a wide range among them (3.7–61.5%). Since “cancer” refers to many different diseases, this wide range is not terribly surprising. In total, 4,243 of 18,650 Covid-19 patients with cancer died, yielding a case-fatality rate of 25.6%. Some of the studies included all types of cancer, while others were more specific (e.g. multiple myeloma only). You can find hyperlinks to each of them here:
A Covid-19 study of 8.26 million adults included 4,053 with Down syndrome. After making allowances for differences in where they live, age, gender, ethnic background, BMI, having dementia, congenital heart disease, and other illnesses which impact the course of Covid-19, the researchers discovered that adults with Down syndrome are five times more likely to need hospitalization and ten times more likely to die from a SARS CoV-2 infection.
People with asthma have fewer ACE2 receptors than those without the disease. Inhaled steroids may further decrease the number of ACE2 receptors which the SARS CoV-2 virus needs to enter a human cell. This likely explains why asthma patients who do get Covid-19 are no more likely to require hospitalization than those without with underlying disease.
AAAAI: Asthma Not Associated With Increased Risk of Hospitalization Among COVID-19 Patients
Ann Am Thoracic: Asthma in COVID-19 Hospitalizations: An Overestimated Risk Factor?
Hospitalization rates roughly follow the pattern for death rates.
CDC: Hospitalization rates per 100,000 population by age and race and ethnicity — COVID-NET
A study conducted in Italy and Spain determined that patients with the blood type A+ were 50% more likely to get sick and too require a ventilator, while the O blood type conferred some protection from Covid-19. The increased severity is likely due to the propensity of blood type A to form blood clots. In one Chinese study, 71% of the patients who died had disseminated intravascular coagulation, a form of abnormal clotting.
How do medications and supplements affect this disease?
MedPage Today reviewed the efficacy of remdesivir, dexamethasone, tocilizumab, anticoagulation, convalescent plasma, monoclonal antibodies, hydroxychloroquine, ivermectin, Vitamin C, Vitamin D, zinc, protease inhibitors, and colchicine.
The Infectious Diseases Society of America (IDSA) periodically updates guidelines for potential treatments for Covid-19. They include critical evaluations of each of the major studies. Currently, their site includes hydroxychloroquine, azithromycin, lopinavir or ritonavir, corticosteroids like dexamethasone, tocilizumab, convalescent plasma, remdesevir, famotidine, neutralizing antibodies, baricitinib, and ivermectin.
Merck, the manufacturer of ivermectin released this statement:
KENILWORTH, N.J., Feb. 4, 2021 – Merck (NYSE: MRK), known as MSD outside the United States and Canada, today affirmed its position regarding use of ivermectin during the COVID-19 pandemic. Company scientists continue to carefully examine the findings of all available and emerging studies of ivermectin for the treatment of COVID-19 for evidence of efficacy and safety. It is important to note that, to-date, our analysis has identified:
- No scientific basis for a potential therapeutic effect against COVID-19 from pre-clinical studies;
- No meaningful evidence for clinical activity or clinical efficacy in patients with COVID-19 disease, and;
- A concerning lack of safety data in the majority of studies.
Merck Statement on Ivermectin use During the COVID-19 Pandemic
Sep 1, 2021 WASHINGTON, DC – The American Medical Association, American Pharmacists Association, and American Society of Health-System Pharmacists “strongly oppose the ordering, prescribing, or dispensing of ivermectin to prevent or treat COVID-19 outside of a clinical trial.”
AMA: AMA, APhA, ASPH Statement on Ending Use of Ivermectin to Treat COVID-19
In late July, the New England Journal of Medicine released the results of a multi-center, randomized controlled trial titled “Hydroxychloroquine with or without Azithromycin in Mild-to-Moderate Covid-19.”
While this study could have been improved by preventing patients and those treating them from knowing whether they were receiving one of those drug regimens or a placebo, it vastly improves our insight into whether these drugs work.
The research showed “A 7-day course of hydroxychloroquine either with azithromycin or alone did not result in better clinical outcomes…at 15 days…Occurrence of any adverse event, elevation of liver-enzyme levels, and prolongation of the QTc interval was more frequent in patients receiving hydroxychloroquine with azithromycin or hydroxychloroquine alone than in those receiving neither agent.”
NEJM: Hydroxychloroquine with or without Azithromycin in Mild-to-Moderate Covid-19
Another randomized, controlled study in mild cases showed a 2% decrease in the amount of the coronavirus obtained from people who received hydroxychloroquine compared to those in the control group after seven days. The difference in the rate of hospitalization for the treatment group and the control group was not statistically significant, nor was the amount of time necessary for symptoms to resolve. The researchers concluded that use of the drug provided no benefit.
Researchers ended a double-blind randomized trial of uninfected healthcare workers taking 600 mg of hydroxychloroquine or a placebo daily for 8 weeks after they discovered no difference in the percentage who developed Covid-19 between the two groups.
A common complain about these studies is that they did not include zinc. Currently, a randomized controlled trial is underway with this combination. It is scheduled for release on December 31st, 2020.
Elderly nursing home residents with adequate concentrations of zinc in their blood were less likely to develop pneumonia. Those who did get sick in that way recovered more quickly. They also needed fewer antibiotics when compared to their peers with low serum zinc concentrations. Therefore, it is likely that zinc alone is protective. A clinical trial to test the efficacy of zinc and/or vitamin C is currently in progress.
Clin Infect Dis: Zinc Supplementation in Elderly Nursing Home Residents
Furthermore, on April 24, 2020, the FDA released a warning against taking chloroquine or hydroxychloroquine. Please be aware that these drugs can have life-threatening cardiac side-effects for 10% of people in the US, and do not attempt to prevent or treat infection by using them on your own.
Hydroxycloroquine also decreases the effectiveness of remdesevir, a drug which improved the clinical course of 65% of severely ill patients in five days.
Gilead Announces Results From Phase 3 Trial of Remdesivir in Patients With Moderate COVID-19
A widely available steroid shows very promising results for extremely ill patients. In a randomized controlled trial of dexamethasone, patients on ventilators who received the drug were one-third less likely to die (29% vs. 41%). Those who received supplemental oxygen were one-fifth less likely to die (22% vs. 25%). People who were not given respiratory support were more likely to die with dexamethasone (17% vs 13%). Consequently, people with Covid-19 should not take this drug unless they are receiving oxygen or mechanical ventilation.
NEJM: Dexamethasone in Hospitalized Patients with Covid-19 — Preliminary Report
Transfusions of blood plasma from people who have recovered from Covid-19 are safe to receive. How effective they are is still being determined, although patients who receive it before severe illness sets in show more improvement.
Mayo: Safety Update: COVID-19 Convalescent Plasma in 20,000 Hospitalized Patients
JAMA: A Randomized Trial of Convalescent Plasma for COVID-19—Potentially Hopeful Signals
A group of researchers conducted an analysis of twenty-three randomized controlled trials. They found that most of the studies had a high risk of bias because patients and health care providers knew whether they were receiving a specific treatment since they did not use placebos. The researchers also addressed the deficiencies in each study. They summarized their findings in this chart:
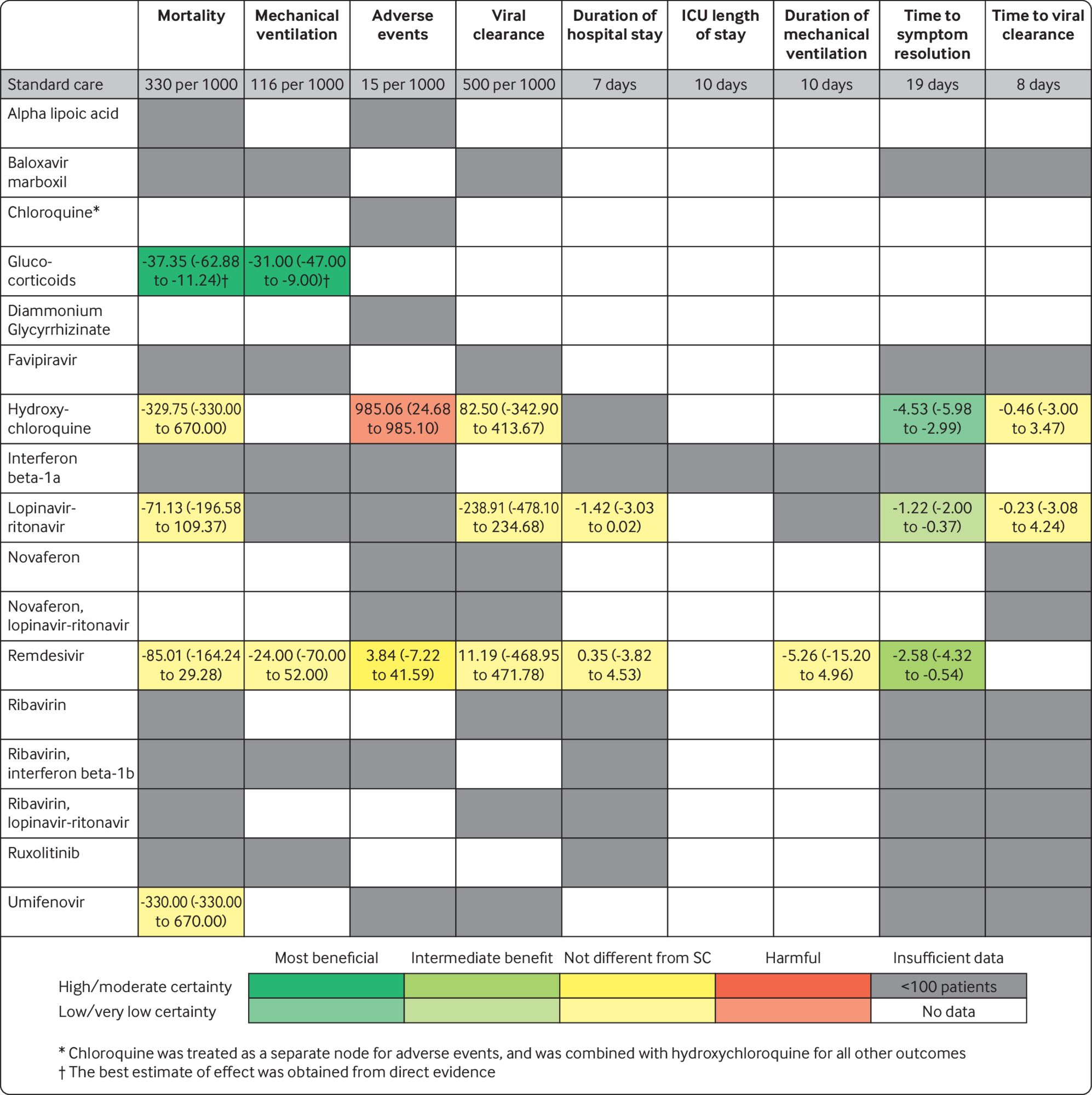
BMJ: Drug treatments for covid-19: living systematic review and network meta-analysis
Researchers have discovered that three common antihistamines inhibit SARS Cov-2 in laboratory testing either by inhibiting the ACE2 enzyme or by binding to another cellular protein. It is important to know that only azelastine appears to provide protection at the recommended dosage. Diphenhydramine (Benadryl) and hydroxyzine (Atarax) require higher amounts than are safe to use.
UF Health: Existing antihistamine drugs show effectiveness against COVID-19 virus in cell testing
Toothpastes and mouthwashes with ingredients which contain a zinc or stannous formula with cetylpyridinium chloride (CPC) are 99.9% effective in inactivating SARS Cov-2 in the mouths of people with Covid-19. Two minutes of brushing teeth or 30 seconds of using a mouthwash prevents viral transmission.
I strongly recommend checking how every supplement you take would affect you if you become infected. You can do this by doing a search with the name of the supplement, the word “cytokine,” and the word “journal.” If you see that what you are using increases cytokine levels, and your doctor has not prescribed it, stop taking it immediately.
Supplements which affect your cytokines will also impact your bradykinins by increasing interluekin-1 and interleukin-6.
Please note that none of these supplements can replace the requirement to protect yourself by frequent and thorough hand washing, social distancing, and wearing a mask.
Oleandrin, a supplement prepared from oleander leaves, does appears to inhibit viral replication. However, it can also easily kill you. Two people had to be hospitalized after eating snails which had ingested oleander leaves. Symptoms of oleadrin poisoning include vomiting and dangerous cardiac abnormalities. When I was studying adverse drug reactions in nursing home patients, the related drug digoxin caused the most severe problems, including death in three patients. Only one of them lived long enough to be included in our study, which required a minimum of one year on-site.
J Am Geriatr Soc: Adverse events related to drugs and drug withdrawal in nursing home residents
Taking a vitamin D supplement appears to boost the protective immunity of people with weak immune systems and decrease the strength of autoimmune reactions. It may help prevent infection and, should the virus establish itself in a person’s body, may decrease the likelihood of the severe reaction caused by a cytokine storm. The Recommended Dietary Allowance is 600 IU for people under 70 and 800 IU for people over that age.
Some research indicates that 30 minutes of summer sun exposure, which also increases vitamin D, is more protective than a supplement.
People seeking treatment for Covid-19 should have their blood tested to determine whether they need additional vitamin D.
A recent study examined 235 hospitalized patients over 40 years old who were infected with SARS CoV-2. Only 9.7% of those with enough Vitamin D circulating in their blood died, compared to 20% of those with a Vitamin D deficiency.
NIH: Vitamin D Fact Sheet for Consumers
NFS Journal: Vitamin D deficiency and co-morbidities in COVID-19 patients – A fatal relationship?
Vitamin C and zinc also appear to protect against infection and to reduce the severity of respiratory infections when they do occur.
Harvard Nutrition: Ask the Expert: The role of diet and nutritional supplements during COVID-19
Zinc decreases the amount of ACE2, the enzyme necessary for the SARS CoV-2 virus spike to enter a human cell. It also limits cytokine storms due to Interleukin-6. Patients with zinc deficiencies experienced more severe complications, longer hospital stays, and increased death rates.
Int J Inf Dis: COVID-19: Poor outcomes in patients with zinc deficiency
Vitamin C also decreases Interleukin-6.In addition, it decreases the amount of Endothelin-1, a powerful amino acid which causes blood vessels to constrict. The researchers recommend a low dose to prevent infection and high doses in severe cases of Covid-19.
However, clinical trials to this point have shown no conclusive evidence of Covid patients improving with the administration of vitamin C.
Nutrition: Vitamin C as prophylaxis and adjunctive medical treatment for COVID-19?
NIH: COVID-19 Treatment Guidelines: Vitamin C
Curcumin, the active ingredient in turmeric, protected patients who contracted the Ebola virus from cytokine storms when it was given intravenously. It should have the same effect in Covid-19 patients. Turmeric alone absorbs poorly in the digestive system. However, formulations with black pepper improve turmeric’s bioavailability by 2000%.
Foods: Curcumin: A Review of Its’ Effects on Human Health
Resveratrol also protects against cytokine storms by inhibiting Interleukin-6.
Pharma & Thera: Therapeutic potential of resveratrol against emerging respiratory viral infections
Melatonin also reduces cytokines. Since the amount of melatonin we naturally produce decreases dramatically as we age, this may factor into the increased severity of Covid-19 in older people. A clinical trial of this supplement in healthcare workers is currently underway.
Sambucol, the active ingredient in elderberries, does help protect against viruses like influenza. Unfortunately, one of the ways it works is by increasing cytokines. That’s what we need to avoid with Covid-19. As of October 10th, there are no published studies concerning elderberries and SARS CoV-2. The FDA has taken action against companies promoting this supplement for Covid-19 prevention and/or treatment.
It is safe to take NSAIDs like ibuprofen and naproxen while sick with Covid-19. In fact, one study found that hospitalized patients who used NSAIDs were 45% less likely to die.
WHO: The use of non-steroidal anti-inflammatory drugs (NSAIDs) in patients with COVID-19
To protect your immune system from the damaging effects of long-term exposure to the stress-induced hormone cortisol, it is important to practice gratitude and develop empathy for others. By shifting your focus to following the precautions of washing your hands and social distancing as a service to help other people avoid Covid-19—rather than doing them from fear of the virus—you will strengthen your immune system’s ability to fight it if you do become exposed.
Mayo: Chronic stress puts your health at risk
Face Coverings and Covid-19
For those of you interested in an in-depth examination of the issues surrounding masks and neck gaiters, I recommend this article:
Cloth Masks to reduce COVID19 transmission
Wear a mask but do not trust it by putting yourself in situations you would avoid if you were not wearing one. Some protection is better than none.
Due to the significant number of infected people without symptoms, the CDC now recommends wearing cloth face coverings in public settings where social distancing measures are difficult to maintain, such as grocery stores and pharmacies. Surgical masks and N-95 respirators should still be reserved for medical personnel.
This is intended to protect other people from you in case you are infected; it will not keep you from getting sick. Scientific evidence does not indicate that this will work well. When wearing a mask, you should never do something you would avoid while not wearing one.
It is extremely important to avoid touching your mask while wearing it. If you do, wash your hands immediately. Children under two should not wear face masks.
CDC: Considerations for Wearing Masks Help Slow the Spread of COVID-19
Mayo: COVID-19: How much protection do face masks offer?
Effectiveness of cloth coverings against particles ranging from 0.02 to 1 µm in a lab. All were near zero for 0.3µm, a size which easily enters the lungs:
T shirt 10% Scarf 10–20% cloth mask 10–30% sweatshirt 20–40% towel 40%
CIDRAP: COMMENTARY: Masks-for-all for COVID-19 not based on sound data
In their June 5th guidance, the WHO advised that cloth masks include three specific layers: an inner cotton layer to absorb fluid; a polypropylene filter in the middle; and an outer layer of non-absorbent material, such as a polyester polypropylene blend.
CIDRAP: WHO unveils COVID-19 mask guidance
While adding a HEPA filter does remove virtually everything down to 0.3µm, smaller virus particles can pass through. Even in a hospital setting, coronaviruses can pass around the edges of filtration systems.
This problem is even greater for people wearing masks which do not form a complete seal on the face.
Effectiveness of N95 respirators and surgical masks designed for eight hours of use in prevention of respiratory virus transmission among medical personnel trained to use them:
N95 respirator 80% surgical mask 80%
After two days of use, the effectiveness of an N95 mask drops to about 50%.
Don’t Use N95 Masks for More Than 2 Days, Research Suggests
AMA: How to Protect Yourself from Counterfeit N95 Respirators
During a pandemic, a one-way valve defeats the purpose of wearing a mask.
What does “flattening the curve” mean? How do we do that?
The initial mathematical model which spurred people into action estimated that doing nothing to prevent the spread of the new coronavirus would result in up to 2.2 million deaths in the United States. In the US in mid-March, the number of new cases was starting to double rapidly. If that continued, we would have had one hundred million American cases by May.
WaPo Simulator: Why outbreaks like coronavirus spread exponentially, and how to “flatten the curve”
Health Affairs: American Hospital Capacity And Projected Need for COVID-19 Patient Care
A flat curve does not mean that we have eliminated the risk, but that the number of new cases per day is not growing. People in the US initially responded to the call to flatten the curve. The goal remains to have fewer people get sick at once to avoid overwhelming our medical system.
I live in Florida. During the first week of March, I moved up my visit to my mother by six weeks to help her gather supplies and to show her how to protect herself. We were not the only ones preparing. Cleaning supplies were so scarce that I almost did not bother to check that aisle when we stopped by the grocery store. An employee was stocking the shelf with six containers of disinfectant wipes. We split them with a woman who was right behind us.
As the number of cases rose in our state, health professionals entreated the governor to impose restrictions. Not until two weeks later, on April 1st, did our governor order a statewide lockdown. Hospitals expected a huge wave of admission which never came. What happened? An analysis of cell phone date revealed that many Floridians did exactly what my family did. We began limiting our exposure without a government order. Sadly, that did not last.
Tampabay Times: How Florida slowed coronavirus: Everyone stayed home before they were told to
A study published on June 8th examined the effects of lockdowns and social distancing in China, South Korea, Iran, France, Italy, and the United States. In those six nations alone, the number of expected cases was off by 62 million. Without intervention, the US should have had fourteen times the confirmed cases that we saw by April 6th, for a total of five million cases. Instead, we reached two million during the second week of June.
The US government is using a model which accounts for social distancing practices in each American state. This model has a state-by-state breakdown of the expected number of deaths; the peak date of each wave; and the number of hospital beds, ICU beds, and ventilators needed during this phase.
Johns Hopkins maintains a worldwide map of diagnosed cases, deaths, and recoveries here. They have recently added a feature which enable you to see what is happening in your county. Go to the upper right of the US map and select your state and county.
The Critical Trends section has several important features:
- Timeline of Covid-19 policies, cases and deaths in your state
- Have states flattened the curve?
- Have countries flattened the curve?
- How did events unfold in Hubei, China?
- Which states have released breakdowns of Covid-19 data by racee?
- Where are Covid-19 cases increasing?
- How is the outbreak growing?
- How does mortality differ among countries?
Johns Hopkins Univ: Covid-19 Dashboard
If you want in-depth information for each state, you can access daily downloads of information from the CDC and DHHS. It is definitely worth bookmarking. Among other information, it includes:
- Number of new cases and deaths in the previous seven days
- Case incidence/Mortality rate/Viral (RT-PCR) lab test positivity in the previous seven days and comparison to the prior seven days
- Hospital admissions in the last seven days and comparison to the prior seven days
- Hospital inpatient/ICU COVID-19 use in the last seven days and comparison to the prior seven days
- Vaccination rates by county (% of total population and % of 65+ population)
- Community transmission level based upon cases and test positivity percentages
- Area of Concern Continuum examining communities in various stages of the epidemic Area of Concern Continuum for counties with rapid rises in cases
Health Data.Gov: COVID-19 Community Profile Report
Most people who recover appear to have immunity for about six months, making spread of the disease less likely once they no longer shed the virus. Reinfection rarely occurs.
CIDRAP: Studies show long-term COVID-19 immune response
CDC: Serology Testing for COVID-19
Covid-19 antibody tests are becoming more widely available. Knowing the sensitivity and specificity of a specific test is extremely important. The FDA determines sensitivity by using samples of a manufacturer’s test on blood which came from a Covid-19 patient. The percentage of those tests which detected the antibodies represents the sensitivity.
Researchers determine the specificity of an antibody test by using blood which was drawn prior to 2020, when there were no known Covid-19 cases in the US. The percentage of tests which did not detect antibodies represents the specificity.
As you can see from this link, there is a wide range of accuracy among tests submitted to the FDA:
FDA: Independent Evaluations of COVID-19 Serological Tests
A combination of the entire population staying home (social distancing), tracing and quarantining entire households where an individual has come into contact with a sick person, placing sick people into isolation except when they require supportive treatment, and closing schools and universities provides the best chance of slowing the infection rate to a manageable level until a more effective treatment or vaccine becomes available.
Univ MI: The Curve is Fattening, Not Flattening. What Can We Do?
Another site enables you to identify which schools throughout the US have reported Covid-19 cases and how many they have:
The Covid Monitor: Tracking cases in every school in the US
This brief video by the Ohio Department of Health provides an excellent object lesson concerning how social distancing works:
OH Dept Health: Flatten the Curve
According to the American Medical Association, the four essentials that must be in place to reopen community facilities and non-essential businesses are: 1) a two-week downward trend in the number of new cases and new deaths; 2) readily available testing; 3) a strong public health system to observe trends and facilitate contact tracing; and 4) hospitals and healthcare workers with sufficient supplies to manage an increased number of Covid-19 patients.
AMA: States should follow 4 signposts to safely reopen America
CDC: COVIDView a Weekly Surveillance Summary of US COVID-19 Activity
As people venture out, public health experts determine what they will do by considering whether an activity is outdoors, which is safer, or indoors; whether they can remain at least six feet apart from others; and how long an activity will take. The longer you remain in one place where people have gathered, the greater the risk.
Before entering a business, they make sure that all employees are wearing masks and remaining six feet away from each other, that hand sanitizer or soap and water is readily-available, and that there are few enough customers to maintain the six foot rule.
They also recommend carrying hand sanitizer with at least 60% alcohol or disinfectant wipes to use whenever entering or exiting a building, avoiding touching your face, and not using public restrooms or water fountains.
Specific guidelines regarding getting haircuts, dining out, attending church services, going to a mall or department store, working out at a gym, visiting a nightclub, socializing in your backyard, attending outdoor events like weddings, going to the beach, camping, staying in a hotel, allowing a friend to use your bathroom, using public restrooms, and participating in sports are discussed here. Note that the level of risk is based upon the people around you practicing social distancing:
On May 19th, the CDC released a sixty-page document with specific three-step guidelines for the reopening of childcare programs, schools and day camps, employers with workers at high risk, restaurants and bars, and mass transit administrators:
The CDC has released guidelines for the use of churches and other places of worship:
CDC: Considerations for Communities of Faith
On June 12th, the CDC posted these guidelines for large group events:
CDC: Considerationsfor Events and Gatherings
What is the difference between social distancing, self-quarantine, and isolation?
Social distancing includes working from home instead of at the office, closing schools or switching to online classes, visiting loved ones by electronic devices instead of in person, cancelling or postponing conferences and large meetings, and enjoying recreation at home or in open spaces in groups of no more than ten people with at least six feet between individuals. For example, you can still walk your dog if you and your pet stay at least six feet away from other people and do not allow your dog to touch someone else’s dog.
In early March, I moved up my visit to my elderly mother by six weeks to help her gather supplies and to show her how to protect herself. I taught her to disinfect counters daily, wash or wipe her hands every time she touched something away from home, and shower at night if she walked out of her gate, even just to get mail.
My second night there, a woman died in her local hospital. We decided getting haircuts was too risky. After gathering supplies at times when we knew few people would be shopping, we treated ourselves with a visit to an antique store we knew would not be crowded. Then, we visited my brother without touching him.
Self-quarantine is for those who suspect they have been exposed. On October 21st, the CDC released a report of a person who worked in a prison. He contracted Covid-19 after multiple short exposures to infected individuals. Therefore, the CDC amended their definition of “close contact” to spending a total of 15 minutes or more within six feet of any person or multiple people who are infectious during a 24-hour period, even if those times are not consecutive.
The current guideline is to remain in quarantine for fourteen days. It involves using standard hygiene and washing hands frequently, not sharing things like towels and utensils, staying at home, not having visitors, and staying at least 6 feet away from other people in your household.
CDC: Public Health Guidance for Community-Related Exposure
Since a possible exposure in mid-March, I have been doing this. The incubation period is 2–14 days, so I bought cleaning supplies and groceries on Days 0 and 1. In addition to educating people about this virus, I have been doing lots of gardening. I am using alternative ways to exercise, rather than going to the gym. Wearing my hair in a ponytail helps me touch my face less often.
Due to increasing rates of infection in our community, I am assuming everyone I meet has been exposed. So, I am repeating the process by remaining in quarantine until Day 14, doing necessary errands on Days 0–1, and returning to quarantine until Day 14.
Infected people must be strictly isolated from others, either at home or in a treatment center. Viral shedding continues for approximately ten days after symptom onset in mild or moderate cases. People with severe cases or with compromised immune systems can remain contagious for up to twenty days.
CDC: Duration of Isolation and Precautions for Adults with COVID-19
Johns Hopkins Univ: Coronavirus, Social and Physical Distancing and Self-Quarantine
How long will this last? What about vaccines?
We really don’t know. It depends upon how quickly enough people can receive an effective vaccine before variants arise which elude the antibodies derived from natural infection or vaccination.
Mayo: COVID-19 variants: What’s the Concern?
Vaccines have been extremely effective at preventing Covid-19:

- For every 147 positive tests, one person was vaccinated
- For every 259 hospital admissions, one person was vaccinated
- For every 167 deaths, one person was vaccinated
To see how I calculated the information in this graphic, click here
Those of you living in the US can click here to access each state’s vaccination web site:
MedPage: COVID-19 Vaccination: A State-by-State List — Starting point to learn who, when, and where
Relying upon herd immunity due to infection in the US is not a good option. Most epidemiologists believe that 70% of the population would have to develop immunity to SARS CoV-2 to prevent most transmission of the virus. To reach 70% of the US population infected with SARS Cov-2, it would take 100,000 new cases per day for 6.5 years (331,000,000 divided by 100,000 times 0.7 divided by 365). Even if that percentage drops to 50%, we would need 4.5 years at that same rate of transmission to achieve herd immunity.
Mayo: Herd immunity and COVID-19 (coronavirus): What you need to know
On Feb. 4, 2021, researchers reported that an algorithm estimated that 71 million Americans had been infected, 2.6 times the number of people with a positive test. That accounts for 21.5% of the US population. Blood donations screened for antibodies in early March 2021 nearly matched that figure.
Health Day: COVID-19 Antibodies Found in One in Five U.S. Blood Donations
It’s helpful to compare Sweden with Norway. As of November 29th, Sweden had 24,074 cases and 662 deaths per million people. Norway had 6,409 cases and 61 deaths per million people. In November, the Swedish Government declared their approach a failure and instituted measures to control the spread of the virus.
WHO: Coronavirus Disease Weekly Epidemiological Update December 1, 2020
BMJ: Covid-19: What Sweden taught Scandinavia for the second wave
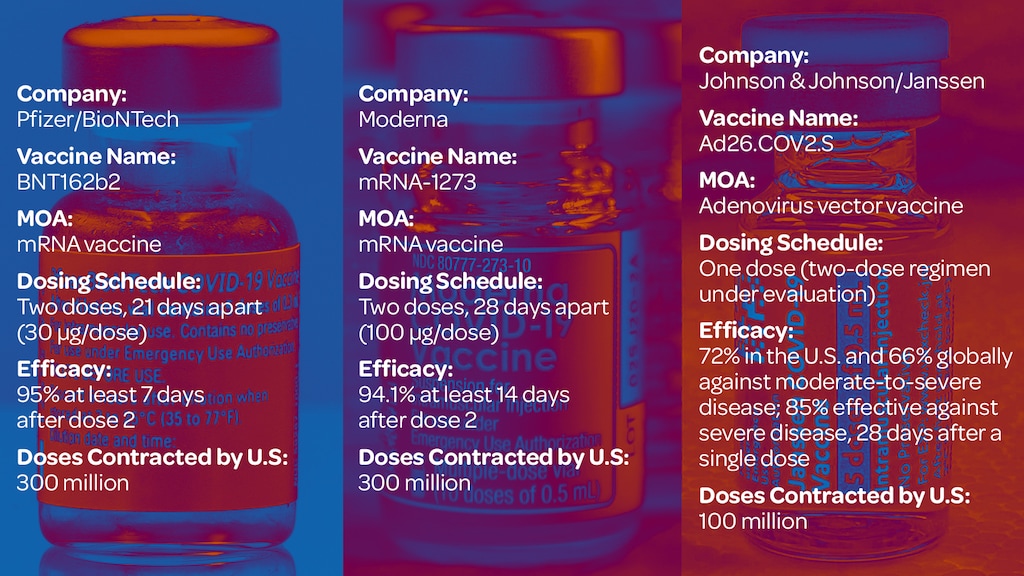
On January 10th, 2020, researchers at Moderna applied existing mRNA vaccine development techniques to the newly sequenced coronovirus genome. Tests indicate the vaccine is safe and produces an immune response in 94% of recipients two weeks after the second dose.
https://www.wired.com/story/moderna-covid-19-vaccine-trials/
Pfizer’s mRNA vaccine has received FDA Approval for people at least 16 years old in the US. For those ages 12–15, the Pfizer vaccine still has Emergency Use Authorization. Two doses are 95% effective two weeks after full vaccination.
The Johnson & Johnson vaccine uses older technology to deliver protection to 72% of recipients in the US after one dose. It protects against 85% of severe cases of Covid-19.
These efficacy rates apply only to those variants which were circulating when each vaccine was in the trial phase. We expect those percentages to drop as new viral strains emerge. Booster shots which incorporate newer variants are already being tested.
A comparison of antibody levels in Moderna and Pfizer recipients revealed over twice the number of antibodies produced by the Moderna vaccine. This is likely due to the increased amount of mRNA in Moderna and the longer interval between doses.
JAMA: COVID-19 Vaccines vs Variants—Determining How Much Immunity Is Enough
JAMA: Comparison of SARS-CoV-2 Antibody Response Following Vaccination with BNT162b2 and mRNA-1273
All the available vaccines contain a portion of the virus’s spike protein; you cannot contract Covid-19 from them.
Here are the CDC’s fact sheets for the Moderna, Pfizer, and the Johnson & Johnson vaccines.
Short-term side effects due to the stimulation of your immune system are quite common, especially pain at the injection site, fatigue, headache, muscle or joint pain, chills, and fever. You should expect a stronger reaction to the second dose. Between the mRNA vaccines, Pfizer tends to produce fewer side effects than Moderna.
The Hill: New study says Moderna vaccine leads to more side effects than Pfizer vaccine
JAMA: Reactogenicity Following Receipt of mRNA-Based COVID-19 Vaccines
A study of two million people compared the likelihood of experiencing a significant Pfizer vaccine-induced side effect to the risk of those same symptoms of Covid-19. Here are the results:

Compared to those infected with SARS-CoV-2, people vaccinated with two doses of the Pfizer vaccine were substantially protected against acute kidney injury, cardiac arrythmia, deep vein thrombosis, hemorrhagic stroke, heart attack, myocarditis, inflammation surrounding the heart, and blood clots in the lung.
While cases of shingles remained rare among individuals in that study, there was an increase in risk among those who received the vaccine.
The Radiological Society of North America recommends waiting 4–6 weeks after the final dose of an mRNA vaccine to undergo a routine mammogram, noting that swelling of lymph nodes in the armpit (lymphadenopathy) is a normal immune response that resolves with time.
This is a side effect which I experienced. While I was aware of a lump for a few weeks, it didn’t cause any problems. Nevertheless, I did mention it to the woman who did my mammogram. She then asked which arms had received the injections in case any swelling appeared in the scans.
NEJM: Safety of the BNT162b2 mRNA Covid-19 Vaccine in a Nationwide Setting
RSNA: Covid-19 Vaccine-Related Lymphadenopathy: What to Be Aware Of
Although no deaths have been attributed to the Pfizer or Moderna vaccines, some people with a history of anaphylaxis or High-Allergy/Mast Cell Disorder have required emergency treatment within 90 minutes of vaccination. This occurs more often in women.
In a recent study, severe reactions occurred in 2.47 recipients per 10,000 mRNA vaccinations. Everyone recovered without going into shock or needing endotracheal intubation.
JAMA: Acute Allergic Reactions to mRNA COVID-19 Vaccines
Severe reactions are less common in the Johnson & Johnson one-dose vaccine. However, six of the 6,800,000 people who received this injection in the US have experienced a very rare severe blood clotting disorder which requires a different treatment than doctors expected. The same reaction to the AstraZeneca vaccine occurs in the UK at a rate of four per million.
Should you develop a severe headache, shortness of breath, and pain in your leg or abdomen within three weeks of receiving the Johnson & Johnson or AstraZeneca vaccine, contact your doctor immediately.
Joint CDC and FDA Statement on Johnson & Johnson COVID-19 Vaccine
This site maintains a list of treatment and vaccine developments:
STAT: Covid-19 Drugs and Vaccines Tracker
Due to their underlying disease and to immunosuppression, cancer patients often show little immune response until after their second dose of a vaccine. That makes adhering to the recommended schedule especially important.
Transplant patients taking immunosuppressants may not develop an antibody response to Covid vaccines. Experts recommend they undergo post-vaccination antibody screening before relaxing the protocols they are using to remain safe.
MedPage: COVID Vax in the Immunosuppressed: Reason for Concern — Discomfiting Results in New Study
What should we do and what should we avoid?
• Wash your hands often for at least 20 seconds. If you must visit a public restroom, use a paper towel to dry your hands, turn off the faucet, and open the door before throwing it away. If using hand sanitizer, use one with at least 60% alcohol.
• Cover your cough or sneeze with a tissue, then throw the tissue in the trash. Do not reuse it.
• Clean and disinfect frequently touched objects. You can use 70% alcohol if necessary.
• Stay home when you are sick.
• Contact a health worker if you have symptoms.
• DO seek emergency care if you have been sick and develop difficulty breathing or shortness of breath, persistent pain or pressure in the chest, new confusion or inability to arouse, and bluish lips or face.
• DON’T touch your face. The virus can enter through your eyes, nose, or mouth.
• DON’T travel if you have a fever and cough or other symptoms.
• DO wear a face covering in public places to protect others in case you are infected without having symptoms but DO NOT trust that it will work.
• DO let people know if you are coughing from an allergy or something else that won’t kill them. • Have a plan in place in case someone in your household develops symptoms and needs to be quarantined at home away from others. • Slowly resume high-risk activities like church services slowly, with a science-based stepwise plan. This one is excellent:
CT: When Your Church Reopens, Here’s How to Meet Safely
“If it looks like you’re overreacting, you’re probably doing the right thing” (Anthony Fauci).
I love the analogy of playing football. You want to place the ball where the other player is going to be, not where he or she is now. Public health works the same way. We anticipate what will happen in the future and act accordingly.
The Hill: Fauci: ‘If it looks like you’re overreacting, you’re probably doing the right thing’
In general, these are sources you can trust:
1) Health Data.Gov – COVID-19 Community Profile Report
2) World Health Organization Situation Reports – These tend to be one day behind. Some nations are not keeping their information up-to-date: WHO: Situation Reports
3) Johns Hopkins University – Johns Hopkins Univ: Coronavirus Resource Center
4) MedPage Today – MedPage Today: Covid -19 Updates
A reflection by Kelly Ladd Bishop, an alumna of Gordon-Conwell Theological Seminary
Schools and gatherings are closing left and right around us. Life will be disrupted for a bit. People will be sick. Hopefully people will also get well! We pray to God for this! God is good.
We cancel gatherings and we stay home, NOT to preserve our own health (although that may be a happy side effect), and NOT because we are afraid, but because we care about those who are vulnerable, who are elderly, who may not have access to health care, and because we don’t want our hospitals overrun, and our doctors unable to help those who need help. This is simple math and science. Fewer vectors, fewer sick people.
What affects “the least of these” affects all of us. Maybe it takes a pandemic to make us realize that we are all on this rock together – doctors, epidemiologists, teachers, students, bus drivers, pastors, babies, homeless people, politicians, weak, strong, all of us.
In my city there is a percentage of the population that experiences food insecurity. Many students receive free meals at school twice a day. When the community closed schools, people began to talk about how to help. A local restaurant gave away free meals today, no questions asked. A group of residents put together a Facebook page offering to pick up groceries or supplies for anyone quarantined (MANY families in our community are currently under quarantine). People have started asking, “how can we help?”
Sometimes life stinks. But when it does, the heart of God can often be seen in those who desire to care for “the least of these,” the vulnerable, the sick, the poor, the scared. Take heart friends, God is always moving. God is moving in our communities. God is drawing us together despite these challenges. God is good, and this will end. And when it does, I pray that we don’t forget the importance of caring for “the least of these,” and that we don’t forget that we’re all in this together.
“‘Then the righteous will answer him, ‘Lord when did we see you hungry and feed you, or thirsty and give you something to drink? When did we see you a stranger and invite you in, or needing clothes and clothe you? When did we see you sick or in prison and go to visit you?’ The King will reply, ‘Truly I assure you that when you have done it for one of the least of these brothers and sisters of mine, you have done it for me.’” (Matthew 25:37–40).
A letter from Martin Luther
During Martin Luther’s second experience with the bubonic plague, he wrote this letter to a pastor struggling with how to respond to the epidemic. For a copy of the entire letter from 1527, click here:
“[Some] sin on the right hand. They are much too rash and reckless, tempting God and disregarding everything which might counteract death and the plague. They disdain the use of medicines; they do not avoid places and persons infected by the plague, but lightheartedly make sport of it and wish to prove how independent they are. They say that it is God’s punishment; if he wants to protect them, he can do so without medicines or our carefulness. This is not trusting God but tempting him…
“Use medicine; take potions which can help you; fumigate house, yard, and street; shun persons and places wherever your neighbor does not need your presence or has recovered, and act like a man who wants to help put out the burning city. What else is the epidemic but a fire, which instead of consuming wood and straw devours life and body?
“You ought to think this way: ‘Very well, by God’s decree the enemy has sent us poison and deadly offal. Therefore, I shall ask God mercifully to protect us. Then I shall fumigate, help purify the air, administer medicine, and take it. I shall avoid places and persons where my presence is not needed in order not to become contaminated and thus perchance infect and pollute others, and so cause their death as a result of my negligence. If God should wish to take me, he will surely find me, and I have done what he has expected of me and so I am not responsible for either my own death or the death of others. If my neighbor needs me, however, I shall not avoid place or person but will go freely, as stated above.’”[1]
[1] Martin Luther, Luther’s Works, Vol. 43: Devotional Writings II, ed. Jaroslav Jan Pelikan, Hilton C. Oswald, and Helmut T. Lehmann, vol. 43 (Philadelphia: Fortress Press, 1999), 119–38, 124.
